You might be wondering why we’re writing about arthritis when we’re in the bone health business. But here’s a statistic that might shock you…
1 in 4 people with rheumatoid arthritis will also develop osteoporosis!
The link is inflammation. And although the research that produced that stat focused on rheumatoid arthritis, all forms of arthritis involve inflammation. You see, “itis” literally means inflammation!
I know firsthand how debilitating it can be. I lived with osteoarthritis for years and even had my right hip replaced because of it.
But eventually, I found a natural approach which has eased the symptoms allowing me to keep my second hip joint without replacement (so far!).
I’ll tell you all about it a little further down the post. But first, did you know that arthritis is the leading cause of disability in America?
It’s true! According to the Arthritis Foundation, more than 300,000 children and 50 million adults suffer from one type of arthritis or another. It occurs more frequently among older people, and women are at a higher risk.
And there are more forms of arthritis than you might expect…
… There are over 100!
Because there are so many types of arthritis, the signs and symptoms can vary from person to person. But a few common joint symptoms include:
-
- swelling
- stiffness
- decreased range of motion
- pain
And more severe symptoms include:
-
- chronic pain
- inability to do daily activities, like walking or climbing stairs
- permanent joint changes, like visibly knobby knuckles
Do you suffer from any of these symptoms?
I know what a painful and frustrating experience arthritis is. But there are many things you can do to ease inflammation and preserve the quality of life and mobility you deserve. And take care of your bone health in the process. The prevention and treatment options differ depending on the type of arthritis though, so let’s take a look at the four main categories first.
Types of Arthritis
As I mentioned, there are over 100 different types of arthritis, so I’ve decided to focus on the four main categories: degenerative arthritis, inflammatory arthritis, infectious arthritis, and metabolic arthritis. And we’ll take a look at the most common types of arthritis within those categories.
Degenerative Arthritis
Degenerative arthritis is synonymous with osteoarthritis.
What is osteoarthritis? Osteoarthritis (OA) is the most common type of arthritis and is the primary cause of disability in older adults. The knee is the most common joint affected by OA.
But osteoarthritis is also common in the hips, spine, toes, and hands. According to the Johnston County Osteoarthritis Project, which is an ongoing population-based cohort study, the lifetime risk of developing OA in the hip is 25% and the lifetime risk of developing OA in the knee is about 46%.
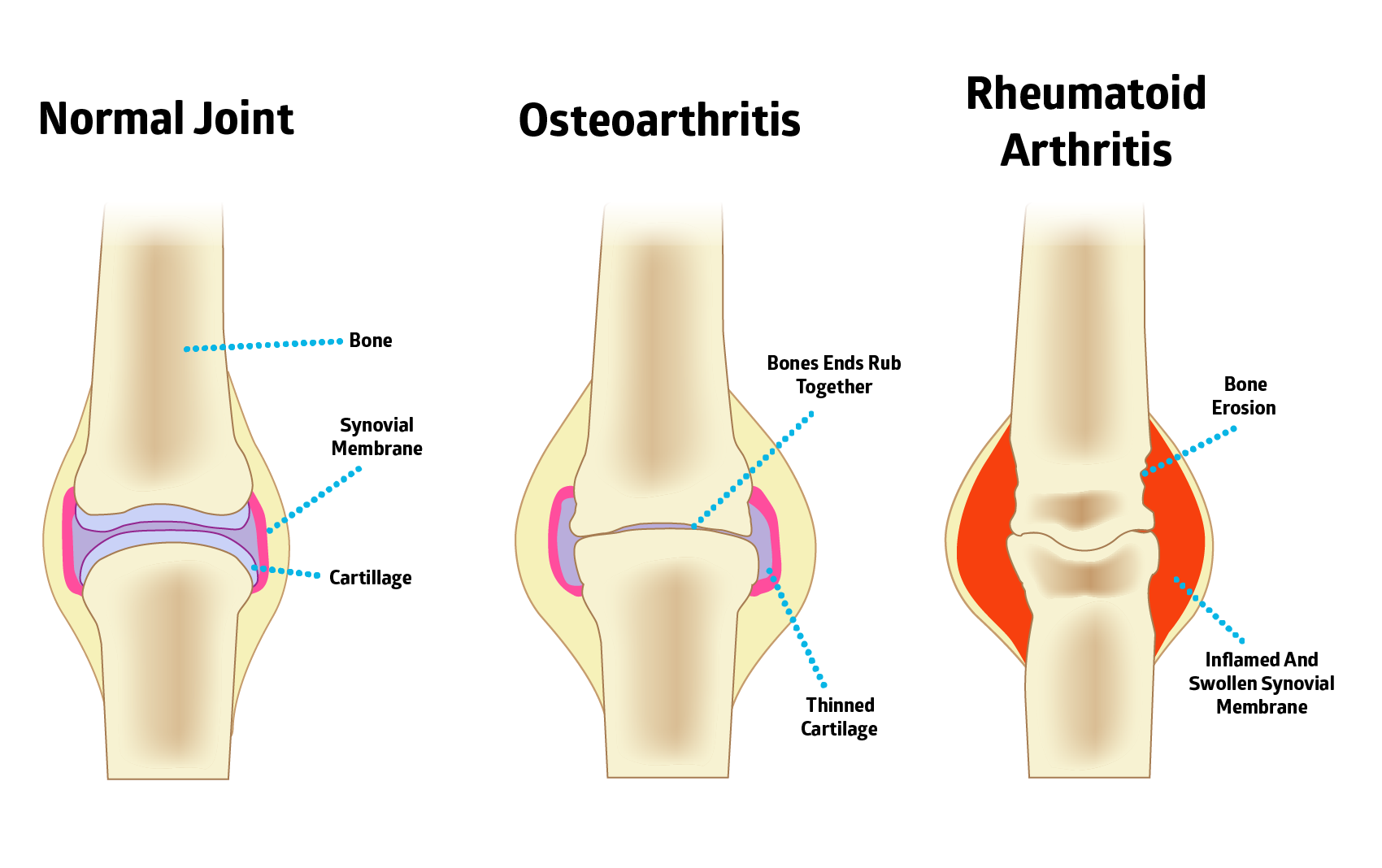
Osteoarthritis occurs when the cartilage that cushions your bones wears down over time. If the cartilage wears down completely, your bones will begin to rub against one another. And trust me, it’s incredibly painful!
Symptoms of OA include:
-
- decreased joint function
- swelling at the joint
- pain and stiffness
- grinding or cracking noise with joint movement
 Inflammatory Arthritis
Inflammatory Arthritis
Inflammatory arthritis refers to a group of diseases caused by inflammation of the joints and other tissues. This includes rheumatoid arthritis and psoriatic arthritis.
Most forms of inflammatory arthritis are autoimmune diseases. Autoimmune diseases occur when your immune system sends inflammation to healthy tissue instead of sending it to fight foreign bacteria and viruses. It’s suggested that autoimmune responses can be triggered by food sensitivities, environmental toxins, and processed foods. Research shows that genetics may play a role too, although it’s not certain that genes alone can determine who develops these diseases.
People with the following may be more susceptible to arthritis and autoimmune diseases:
-
- Compromised vitamin D receptors (VDR). These receptors allow the body to respond to vitamin D.
- Damaged mitochondrial manganese superoxide dismutase (MnSOD) genes. This gene is important to the use of manganese and helps destroy free radicals.
- Ineffective pyridoxamine 5′-phosphate oxidase (PNPO) genes. This gene helps produce the enzyme responsible for breaking down vitamin B6 so we can absorb magnesium.
Other potential factors may include hormones, stress, smoking, and infectious agents.
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is the most common type of autoimmune arthritis and affects more than 1.3 million Americans. Of those affected by rheumatoid arthritis, 75% are women.
RA is not a degenerative disease caused by wear and tear like osteoarthritis. It’s caused primarily by excess inflammation. Special enzymes signal prostaglandins (lipids that play a key role in the generation of the inflammatory response) in your body to band together and inflame your joints. And remember, chronic inflammation activates your bone-resorbing osteoclasts, leading to excess bone loss.
Despite being common, RA is currently considered a condition without a cure. Most treatment options only help ease symptoms of the disease or affect its progression. It’s not known for sure why some people’s immune system stops working as it should. But possible causes include genetics and exposure to a trigger, like fighting an infection.
Symptoms of RA include:
-
- low-grade fever
- weight loss
- anemia (shortage of blood cells)
- low energy
- joint pain and stiffness in the morning or when getting up after a long rest
- rheumatoid arthritis nodules — firm lumps of benign tissue that grow under the skin
What is psoriatic arthritis?
Psoriatic arthritis involves joint inflammation and typically occurs in combination with the skin disorder psoriasis.
Psoriasis is a chronic inflammatory condition that affects approximately 2–3% of the world’s population. And 30% of those people with psoriasis will eventually develop psoriatic arthritis. Psoriatic arthritis has also been associated with celiac disease and gluten sensitivity, as well as zinc deficiency.
Symptoms of psoriatic arthritis include:
-
- stiff joints with swelling, redness, and heat
- swelling and redness in the hands, fingers, or toes
Infectious Arthritis
Infectious arthritis, also known as septic arthritis, is categorized as inflammation of a joint caused by infection. Large joints like the hip or knee tend to be susceptible, but it can also affect other joints.
Infectious arthritis is typically caused by a virus, bacteria, or fungus. Streptococcus (strep throat) and Staphylococcus (staph infections) are both common causes. It can also be caused by contamination of an open wound or through surgical procedures like knee surgery. Septic arthritis can also be contracted through food poisoning, sexually transmitted diseases, and blood-to-blood infections through transfusions or shared needles.
Symptoms of infectious arthritis include:
-
- fever
- chills
- weakness and fatigue
- pain of affected joint, especially when in use or moving
- swelling
- warm to the touch and red
Most people will make a full recovery with a combination treatment that includes draining the infected fluid from the joint, and antibiotics which can resolve the infection. Antibiotics are typically administered immediately to avoid the infection from spreading. However, sometimes it can become chronic. Chronic septic arthritis, while less common, is caused by organisms including Candida albicans and Mycobacterium tuberculosis.
Metabolic Arthritis
You may know metabolic arthritis as gout or gouty arthritis. It occurs in about 4% of the US population. It’s most common in older men, but also occurs in post-menopausal women, and those who;
-
- are taking diuretics (water tablets)
- have high cholesterol levels
- are overweight
What is gout? Gout is an inflammatory type of arthritis caused by high uric acid in the blood, which causes uric acid crystals to form in joints. These cause very painful attacks and when recurring, can cause permanent joint damage.
There are several stages of gout: asymptomatic hyperuricemia, acute gout or a gout attack, interval gout, and chronic gout.
Symptoms of gout include:
-
- pain and swelling in joints, particularly the big toe, knees, elbows, wrists, and fingers
- swelling, heat, redness at the joint
- painless lumps called tophi that develop under the skin around the joints
- kidney stones
 Arthritis Prevention
Arthritis Prevention
As you now know, there are more than 100 types of arthritis and each comes with its own set of risk factors. Some are within your control, and others aren’t. Gender and genetics play a big role in your likelihood of developing arthritis, but fortunately, there are plenty of ways you can limit the risk.
A few types of arthritis with modifiable risk factors are:
-
- Osteoarthritis: Keep OA at bay by maintaining a healthy body weight. Excess weight is one of the biggest risk factors when it comes to osteoarthritis because extra weight places additional pressure on weight-bearing joints. Diabetes may also be a risk factor for OA. Recent research suggests that it can trigger systemic inflammation that leads to cartilage loss, according to the Arthritis Foundation.
- Rheumatoid Arthritis: Avoid the onset of RA by quitting smoking, eliminating allergenic foods from your diet, and avoiding other toxic triggers as these are a few known risk factors of RA.
- Gout: Maintain a healthy diet low in alcohol, sugar, and purines, which are natural substances found in foods that contribute to the production of uric acid. A few examples are liver, kidneys, sardines, and mussels.
Researchers are still trying to fully understand the causes and mechanisms behind these conditions. However, many types of arthritis are thought to be a result of an environmental trigger or a genetic predisposition.
Take some time to discover your personal arthritis triggers. Even with a genetic predisposition, there may be avoidable environmental triggers contributing to your symptoms.
Arthritis, Inflammation and Bone Loss
Your bone density depends on two opposing forces at work deep inside your bones. Building new bone and resorbing old bone are both critical to the remodeling process, which is ongoing throughout your life.
In bone remodeling, osteoblast cells build bone, while osteoclasts break down bone.
As you age, the process becomes unbalanced. Your osteoclasts break down worn-out bone at a quicker rate than your osteoblasts form new bone. This explains why after peak bone mass, around age 40, you lose about 1% of your bone density each year.
And anything that promotes inflammation (like arthritis), also promotes osteoclast activity, which causes extra bone loss.
Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce inflammation that accompanies arthritis. Especially among rheumatoid arthritis sufferers. NSAIDs include your typical bathroom cupboard pharmacy standbys like aspirin (Bayer), ibuprofen (Advil), and naproxen (Aleve). And with the exception of aspirin, all the NSAIDs, interfere with the resolution of inflammation.
They may be effective at masking joint pain, but they rarely eliminate the inflammation causing that pain. And even worse, they can trigger serious side effects throughout your body. There are volumes of studies and research papers on this topic. Some of the unnerving revelations include serious cardiovascular risks, like high blood pressure, edema, and even heart failure.
Even more prevalent are the gastrointestinal side effects related to NSAIDs. Upper and lower gastrointestinal bleeding is just one particularly unsettling example.
In addition to greatly increasing these risks, they also promote bone loss. How? NSAIDs keep inflammation going. Plus, they impair gastrointestinal tract, cardiovascular, and liver function.
A properly functioning digestive tract is required both for the effective release of nutrients from our food and for our ability to absorb these nutrients. Whether they were released from the food matrix or a supplement.
Once nutrients are absorbed from our digestive tract, they travel via the portal vein to the liver and from there are sent out into the bloodstream for delivery through our vasculature (blood vessels and heart) to our bones and the rest of the body.
When the vasculature is compromised, so is our blood flow. As is our ability to deliver both oxygen and nutrients to our cells.
Insufficient oxygen delivery increases the production of free radicals, increasing inflammation. And just as you can’t make an omelet without eggs, you can’t build bones without the delivery of the nutrients they require.
NSAIDs have also been connected with inhibited bone healing. So while they may help ease the pain of arthritis, anyone with bone loss or who recently suffered a fracture should be especially wary of taking NSAIDs for pain management.
To avoid this bone-damaging inflammation, I recommend incorporating anti-inflammatory foods and other lifestyle changes like exercise, which I’ll discuss further below.
If you must take an NSAID to manage chronic pain, take aspirin, at the lowest dose possible.
5 Natural Arthritis Remedy Options
Now, if you happen to like all things natural, you can try the following remedies to reduce inflammation and ease arthritic symptoms.

Stay Active
Despite concerns that aerobic and strengthening exercises may exacerbate joint symptoms in those with osteoarthritis and rheumatoid arthritis, research indicates otherwise. In fact, exercise actually helps to increase blood flow, bringing in nutrients and expelling waste.
Stretching, strengthening, and aerobic activity not only help you fight through stiffness, but also increase muscle strength and cardiovascular fitness.
Tai chi, in particular, has been shown to maintain and improve health and relieve pain. Arthritis foundations all over the world are supporting tai chi as a natural and effective treatment option, thanks to the following scientific research.
A 2003 randomized clinical trial published in the Journal of Rheumatology had older women with osteoarthritis complete three months of a sun-style tai chi program made up of 12 movements. This program was specifically developed to reduce symptoms and improve physical function of arthritis patients. The results? The women were able to safely perform the 12 movements and their balance, abdominal strength, and arthritic symptoms improved!
And the Journal of Advanced Nursing and Arthritis Care and Research have also published similar findings.
But so far, the largest tai chi for arthritis study was presented in 2010 at the annual Scientific Meeting of the American College of Rheumatology. This landmark study had 354 participants randomly assigned to two groups, where they all received baseline and follow up evaluations after eight weeks. Reports of physical function, pain, fatigue, and stiffness were all collected at baseline and at the final evaluation. This included questions on their ability to perform daily activities, their perceived self-efficacy, and overall general health. Plus, physical performance measures, like timed chair stands, balance testing, and gait speed.
The intervention group immediately received tai chi lessons for eight weeks, while the other group was a delayed control group who waited for classes, but did eventually receive the tai chi course after the control group completed their eight weeks.
The results at the end of the eight weeks showed that the participants who received the intervention reported moderate improvement in stiffness, fatigue, and pain. They also had an increase in balance and reach, and an overall sense of wellbeing.
For more on tai chi and how it can benefit your bones, head to our post: Tai Chi for Osteoporosis.

Maintain a Healthy Weight
This is especially important for those suffering from osteoarthritis as being overweight can lead to more joint pain and disability. Maintaining a healthy weight can lighten the load that is placed on your hip joints and knees.
Exactly how excess weight affects osteoarthritis is still unclear, but John Hopkins Arthritis Center states that even being 10 lbs overweight can increase the force on your knee by 30–60 lbs each step! Overweight women increase their risk of knee osteoarthritis by 4x and men increase their risk by 5x. So excess weight and obesity shows a consistent link to knee osteoarthritis.
The good news is, the Framingham Study showed that elderly people — both men and women who lost enough weight — could decrease knee osteoarthritis and reduce pain. That means weight loss can be an important modifiable factor in the treatment of knee osteoarthritis.
There is also evidence that excess body weight is a risk factor for the development of rheumatoid arthritis.

Improve Your Sleep
About 70% of people with osteoarthritis experience sleep disturbances that can range from waking up earlier than desired to problems falling or staying asleep.
Pain can be a cause of these sleep disturbances, but it may work both ways. Researchers suggest that a poor night’s sleep can make it more difficult to cope with pain the next day, which can turn into a nasty cycle of poor sleep and pain magnification.
While everyone is different, the following may help you get a more restful sleep:
-
-
- Heat therapy — ease your joint pain by using a heat pad for 15 or so minutes before bed. Taking a warm, soothing bath with mineral salts may also help.
- Stretch and exercise — discussed above, moving your joints can reduce stiffness and pain, and make it easier to sleep at night.
- Anti-inflammatory diet — your dietary choices can play a role in easing your arthritic symptoms. Anti-inflammatory foods like omega 3 fatty acids in fish and fish oil, turmeric curcumin, and ginger can help ease symptoms and spice up your diet.
- Control your surroundings — establish a nighttime routine that avoids caffeine, large meals, TVs, and bright-screened electronics, and get into a habit of going to bed around the same time every night.
-

Anti-inflammatory Diet
As discussed earlier, all types of arthritis involve inflammation. This can exacerbate symptoms, making it difficult to cope with pain. And remember, it also negatively affects your bones.
To combat this, we recommend adding the following three anti-inflammatory heavy hitters to your diet. They are boron, ginger, and turmeric. And you should seriously consider fish oil too. It’s so important that I’ve written a whole section on it a little further down.
Boron
When you think of anti-inflammatory nutrients you probably don’t think about the trace mineral boron, but now you will! One of the benefits of boron is that it has plenty of anti-inflammatory properties and has shown promising results when it comes to controlling inflammation associated with osteoarthritis and bone mineral density.
Boron does this by limiting the release of certain chemicals that leak into your joints causing the swelling and pain you may experience.
Case reports, epidemiological evidence, and controlled animal and human trials have provided evidence for the use of boron as an effective and safe treatment for OA.
Lara Pizzorno, our Bone Health Expert, was telling me that her husband Joe was suffering from such severe knee osteoarthritis last summer that he had to stop playing basketball.
Over the last year, he’s taken 6 mg of boron daily (along with his excellent diet and other foundational supplements) and it’s made a huge difference. Lara reports he’s even back to playing basketball again!
Now, this is just one piece of anecdotal evidence and does not replace science-based research. But I think sometimes it’s nice to hear first-hand stories in addition to the solid research that has already been conducted. For more on this trace mineral, check out Boron Uses and Health Effects.

Ginger
Ginger contains phenolic substances called gingerols. 6-Gingerol is the active component of ginger and has anticancer, antioxidant, and anti-inflammatory properties. It’s also been studied in Arthritis and Rheumatology to reduce knee pain in patients with osteoarthritis.
This randomized, double-blind, placebo-controlled study followed 247 patients with moderate-to-severe osteoarthritis of the knee for six weeks. Patients were given ginger extract or a placebo twice daily (the option of acetaminophen (Tylenol) was allowed as a rescue medication). The results showed that the ginger extract group showed significant reduction in symptoms of osteoarthritis of the knee based on the self-assessment of “knee pain on standing”.
While ginger extract is an option, you can also incorporate ginger into your diet the following ways:
-
- Ginger powder — wonderful in curries.
- Ginger tea — freshly sliced and steeped with lemon. Tip: You can also freeze organic ginger and grate it (with skin on) into your tea. This way your ginger doesn’t spoil and is always available when you want it!
- Fresh ginger — in juices, smoothies, or savory recipes.

Turmeric
Turmeric is an ancient spice traditionally used in Indian and Ayurvedic medicine. Recently, it’s shown its therapeutic value in thousands of studies on human diseases. More than 600 diseases to be precise!
Curcumin, the active agent in turmeric, boosts antibacterial, antifungal, anticancer, antiviral, antioxidant and anti-inflammatory properties. In fact, a study published in The Journal of Oncogene showed that curcumin is more potent than NSAIDs like aspirin and ibuprofen when it comes to suppressing inflammation and blocking the process of tumor cell proliferation.
In other words, it can help relieve inflammation and pain safely and naturally compared to over-the-counter and prescription drugs.
Bonus: You may also be surprised to know turmeric’s active ingredient is now linked to supporting bone mineral density.
Researchers from Genoa University studied 57 adults with osteopenia. These otherwise healthy adults had an average age of 70. Twenty-eight of them received a control treatment while the other 29 received an oral curcumin supplement (1,000mg of curcumin).
Besides that, all 57 followed the same weekly protocol. The protocol included taking calcium, vitamin D and C, and exercising for 20 minutes, four times a week.
The researchers tracked the participants’ upper jaws, heels, and pinky fingers over 24 weeks using an ultrasound method.
Now to be fair, this was a small study, and an ultrasound is not the gold standard for measuring bone density like a DEXA scan is. I’d prefer to see results for a longer term than four months and to see another higher quality study verify the results, but it looks pretty promising all the same.
At the 24 week mark, the curcumin group saw 7.1% and 4.8% bone density increases in their small fingers and upper jaws, respectively. And the control group? They saw no significant changes in any of the three measured bones.
Want to incorporate this anti-inflammatory root into your diet? Try our delicious recipe below.
Discover more anti-inflammatory foods in our post: Top 5 Effective and Natural Remedies for Inflammation.
Fish Oil
Omega 3 fatty acids found in fish oil are shown to be a natural treatment for many diseases.
Researchers found positive therapeutic results for inflammatory and autoimmune diseases like Crohn’s, psoriasis, ulcerative colitis, multiple sclerosis, and even migraines. The two key omega 3 fatty acids are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), and while each has its own special beneficial effects, they both reduce cellular inflammation.
Omega 3 fatty acids and fish oil have been shown to have therapeutic effects on rheumatoid arthritis. In one double-blind, placebo-controlled study, 66 patients with rheumatoid arthritis were given fish oil or a placebo for up to 30 weeks.
After 30 weeks, many of the fish oil patients were able to stop taking NSAIDs. And they did so without experiencing increases in arthritic flare-ups. Those taking the fish oil experienced significant improvements in their joint pain, morning stiffness, and even the pain measured by their physicians. Those taking the placebo saw “no clinical parameters improved” from their initial joint pain baseline.
A nested case-control study found that low omega 3 fatty acids were associated with an increased risk for development of rheumatoid arthritis.
The study’s main takeaway is ensuring EPA/DHA adequacy may help prevent the development of rheumatoid arthritis in those with a genetic predisposition.
It doesn’t stop there, though. One study showed 1,000–2,000 mg of fish oil a day had “significant efficacy” in improving knee performance in patients with knee osteoarthritis.
The best food source for omega 3 fatty acids is coldwater fish, including mackerel, salmon, and sardines. But the reality is, most people are not getting enough through diet alone.
Typically, people will supplement with a high-quality fish oil to ensure they are getting clinical doses to reap the benefits.
If you think plant-based omega 3 fatty acids from alpha-linolenic (ALA) are your answer, think again. Less than 5% of ALA is converted to EPA and less than a 0.1% is converted to DHA. So in terms of benefits for heart health, cognitive function, and arthritis, go straight for oil options with EPA and DHA.
For me and my osteoarthritic hip, fish oil seemed to be a no-brainer. But I ran into the same problems with every omega 3 fish oil I tried.
Gross fish burps and indigestion, bulky pills to swallow, and the fact I never really knew where the fish was harvested. It was also really difficult to know if I was taking enough to make a difference.
This became a cause near and dear to my heart (and my angry hip). I realized there was huge potential to come up with a solution to all this. And after 2.5 years of researching, testing, and developing, I finally found a delicious solution!
It’s top shelf omega 3 fish oil that delivers 750 mg of EPA and 450 mg of DHA in each great tasting tablespoon, plus 280 mg of other healthy omega 3s. It also contains two potent antioxidant and anti-inflammatory nutrients, astaxanthin and turmeric curcumin. These antioxidants help support your body’s natural, healthy inflammatory response. We call it Triple Power Omega 3 Fish Oil. And I guarantee you’ll absolutely love it.
I’ve been taking it for a while now and can confidently report it’s done wonders for my joint pain. Morning wakeups are no longer the torturous chore they once were. If you’ve already had a taste of Triple Power, let me know what you think in the comments below.
[ac_banner name=”fishdelicious”]
What You Need to Know About Your Arthritis
Are you one of the 50 million adults in America suffering from arthritis?
If you’ve been diagnosed with arthritis of any kind, you’ve probably scoured the internet and spoken to several healthcare professionals for managing or treating it.
For me, committing to a regular exercise program and keeping my diet focused on clean, healthy, and anti-inflammatory foods has done wonders for the arthritis in my hip.
But the most important management system is you! Arthritis affects everyone differently, so learning and maintaining what helps you thrive and live well is crucial.
Do you have any recommendations for me or the rest of the AlgaeCal family? If so, I’d love to hear them in the comments below.





Lynn
June 30, 2018 , 8:47 amAre your vitamins FDA approved, as others are not? If they are so great, why not sell them in stores?