Did you know about 1 in 4 men will break a bone due to osteoporosis after age 50?
How about that roughly 2 million American men have osteoporosis… with another 12 million at risk of developing it?
Sure, women are more likely to get osteoporosis, but men certainly aren’t immune. In fact, men get osteoporosis for much the same reasons as women.
How Do Men Get It?
Like with women, age plays a role in male osteoporosis.
After peak bone mass (around age 40) both men and women begin to lose about 1% of their total bone mineral density each year. Women tend to develop osteoporosis much earlier in life, usually in their fifties, because of menopause. The drop in estrogen production at this time increases bone loss to as much as 5% or even 10% each year in some women!
So while men are not experiencing this rapid rate of bone loss in their fifties, by age 65 or 70 men and women lose bone mass at the same rate. At this time, the absorption rate of nutrients and foods decreases in both sexes. This can cause excessive bone loss and lead to increased fracture risk.
In fact, the numbers show that:
- One in four men over age 50 will break a bone due to osteoporosis.
- Men older than 50 are more likely to break a bone due to osteoporosis than they are to get prostate cancer.
- Men with osteoporosis are more likely to die within a year of breaking a hip (from complications related to the break) than women.

Causes of Osteoporosis in Men
There are many risk factors for, and causes of, osteoporosis in men.
But in general, osteoporosis in men is an indication that something else is going on.
And for many men, that “something” is hormonal.
#1 Drop in Hormone Levels: As you know, we gradually start to break down more bone, more rapidly as we age. This is partly due to decreased levels of estrogen and testosterone.
The most common cause of osteoporosis in men happens to be testosterone deficiency. That’s because a small amount of testosterone is converted to estrogen in men. So a drop in testosterone levels also leads to a drop in estrogen levels. And estrogen is critical to bones. Why? It plays an important role in the growth of bone and its maturation. It also regulates healthy bone turnover.
#2 Deficient in Bone-Building Nutrients: Older adults absorb calcium less efficiently than children. Especially from the intestine and kidneys. This means that if you’re not giving your bones what they need in terms of vitamins and minerals, your bones will start to lose bone density.
Calcium is critical to bone health – you already knew that. But did you know that in addition to calcium, there are 12 other minerals and three vitamins that are essential to healthy and strong bones? So as you age and your ability to absorb nutrients decreases, it’s more important than ever to give your bones what they need in their proper proportions. Discover the top bone-building nutrients and how to get them here.
#3 Lack of Weight-Bearing Exercise: When it comes to bone health, nutrition is key, but so is exercise. A lack of exercise, specifically weight-bearing exercise, plays a vital role in deteriorating bone health.
Weight-bearing exercise is an exercise where you ‘bear your own weight’ and is one of the best things you can do to increase your bone strength. If you don’t regularly stress your muscles, joints, and bones, they begin to weaken over time. But when it comes to osteoporosis in men, some exercises appear to be more beneficial than others. A five-year study conducted by the Centre for Bone and Arthritis Research discovered that when it comes to protecting men’s bones, the superior sports are:
- Basketball
- Volleyball
- Jogging
- Soccer
See how all these sports are ‘weight-bearing’? The study showed that these sports reduced a man’s risk of developing osteoporosis later in life. This study suggested that spending just four hours per week playing a weight-bearing sport helped the men increase their hip bone density by as much as 1.3% over the period of the study. This was especially critical when viewed against the discouraging data of sedentary men who lost as much as 2.1% of their hip bone density over the same period.
#4 Medical Conditions: There are two main types of osteoporosis: primary and secondary. Primary osteoporosis refers to age-related osteoporosis or an unknown cause. Secondary osteoporosis, on the other hand, refers to bone loss caused by certain lifestyle behaviors, diseases, or medications.
Unfortunately, there’s a long list of medical conditions or diseases that lead to low bone mass. They range from conditions such as diabetes and cystic fibrosis to blood disorders such as anemia. If you’re concerned about a medical condition causing bone loss, discuss it with your healthcare provider. And if you have a chronic condition and have been taking medication for some time, it’s even more crucial to focus on diet and exercise.
#5 Medications: If you’re taking medication, it may contribute to bone loss. This link provides information on several classes of medications that may cause bone loss, but it isn’t a complete list. If you’re concerned about a medication causing bone loss, please discuss it with your healthcare provider.
#6 Lifestyle Factors: There are some things you can’t control when it comes to your bone health. Your age, genetic predisposition, or gender. But you can control your lifestyle. And there are certain lifestyle factors that contribute to bone loss.
It’s no secret that smoking is associated with lung cancers and cardiovascular diseases, but studies show that it also affects your bones. A majority of the studies conducted to establish a link between smoking and bone health have had a few common findings:
- The longer someone smokes, the greater their chance of a fracture later in life.
- Older men and women who smoke have significantly more bone loss than those who don’t in the same age group.
- Fractures, when they do occur in smokers, take longer to heal compared to fractures in non-smokers.
- Compared with nonsmokers, women who smoke often produce less estrogen and tend to experience menopause earlier, which may lead to increased bone loss.
Another lifestyle factor that may contribute to bone loss is consuming excess alcohol. Particularly, 3 oz (3 glasses) or more per day has been shown to negatively impact your bones. On the other hand, research shows that moderate alcohol consumption (1-2 glasses per day), particularly wine, may actually benefit your bones.
So the takeaway is, enjoy that glass of wine at dinner, but don’t overindulge regularly. For more, see our post on Alcohol’s Effects on Your Bones.
Further lifestyle factors include little or no exercise and a lack of bone-building nutrients (discussed above).
#7 Sleep Deprivation: Getting your Zzzz’s is no joke. Researchers have shown that a lack of sleep in rats can halt bone formation and decrease bone density. They suggest that this can also be true in humans. Sleep deprivation can affect how your bones repair themselves. The National Sleep Foundation recommends that adults (ages 26-64) get 7-9 hours of sleep and that older adults (65+) get 7-8 hours of sleep.

Where Do Men Get Osteoporosis?
The common areas of osteoporosis are in the hip, femur, and spine/vertebrae, and wrists for both men and women. But after age 75, the incidence of hip fractures in men sharply increases. And in the first 12 months after a hip fracture, men have a higher mortality rate than women.
Vertebral fractures are also more common in men under the age of 50, but after 50, vertebral fracture incidence is higher in women.
While these areas (hip and vertebrae) have a higher incidence depending on age, men can get osteoporosis in all of the common osteoporosis area sites. Men (and women) can also get osteoporosis in other areas too, such as the forearm and shoulders.
The Difference Between Male and Female Osteoporosis
When it comes to bone mass, there are gender differences.
During adolescence, the different musculoskeletal effects of testosterone and estrogen in males and females begin to emerge.
In males, muscular and skeletal developments during puberty is due to increasing levels of testosterone and IGF-1 (insulin-like growth factor, which plays a role in bone growth and development). This results in increased muscle mass and strength.
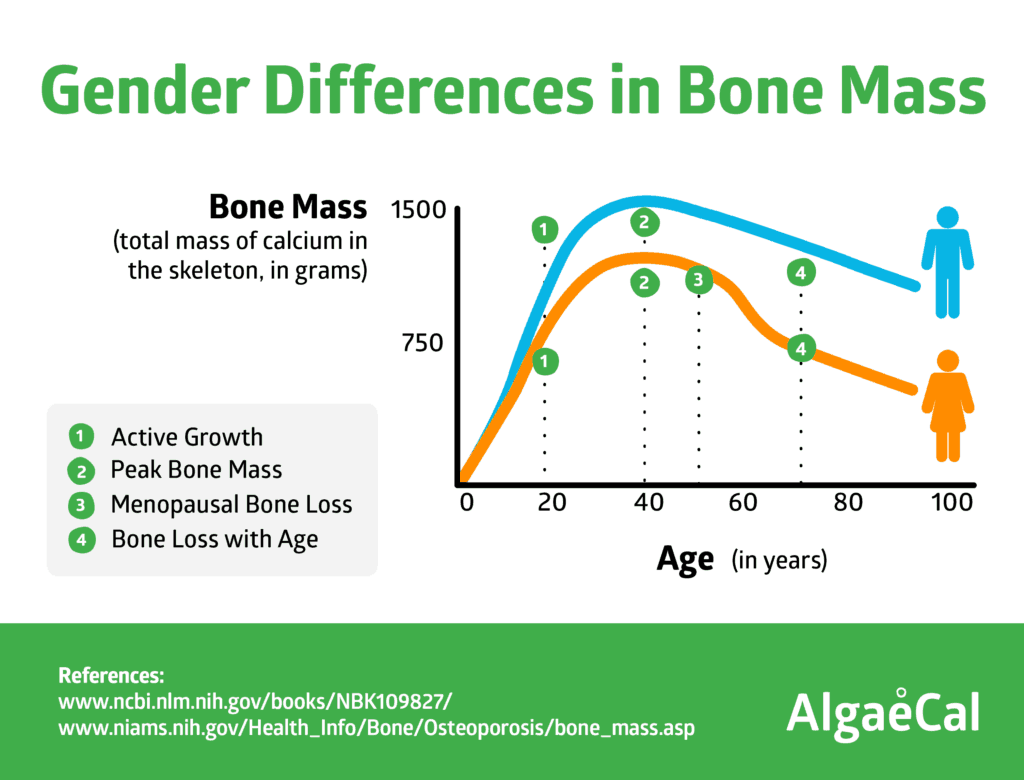
[embed_infographic title=”Gender Differences in Bone Mass” alt=”Gender Differences in Bone Mass” src=”https://blog.algaecal.com/wp-content/uploads/gender-differences-in-bone-mass.png”]
Why is this important?
Because skeletal fragility in old age is related to peak bone mass in young adulthood.
The more bone mass you accrue when you’re younger, the better your chances of reducing your risk of osteoporosis later in life. And males tend to accrue a higher peak bone mass.
This is due to the fact that before puberty, males and females gain bone mass at similar rates. But after puberty, males tend to acquire more bone mass.
A study examining 373 women and 323 men (age 20-97 years) assessed gender difference in bone geometry and volumetric BMD in the lumbar spine, femoral neck, distal radius and distal tibia.
The study showed that men had 35-42% larger bone areas than women. And while bone area increased equally over life in both sexes, men increased more in peripheral sites.
The takeaway?
Age-related bone changes are complex. But because men generally have a higher peak bone mass it may explain in large part why fragility fractures are more common in elderly women than elderly men.
Risk Factors
There are many risk factors for osteoporosis such as gender, diet, hormones, and physical activity. Factors that are linked to an increased risk in men include but are not limited to:
- Family History: Having a family member with osteoporosis puts you at greater risk as osteoporosis is genetic.
- Certain Medications
- Poor Lifestyle Habits: Such as smoking, lack of sleep, low calcium intake, and inadequate exercise can increase your risk of fragility fracture.
- Race: Caucasian men seem to be at a higher risk of osteoporosis. Although all men can develop osteoporosis.
- Chronic Diseases: Such as diabetes, anemia, low testosterone levels, hyperparathyroidism can lead to bone loss.

Bone Density and Signs of Bone Loss
Bone density or bone mineral density is the amount of bone mineral in your bone tissue. Healthy bone looks compact and strong, while bones with osteoporosis are spongy and weak.
To measure your bone density, the gold standard test is called a DEXA scan, which I’ll discuss in the section below.
While osteoporosis has many risk factors like the ones above, there are few obvious signs or symptoms, making it difficult to pinpoint.
But there are a couple of physical signs of bone loss.
- Wrinkles. Or what some people call their life or lifelines. By simply using a mirror and looking at the depth of your face and neck skin wrinkles, researchers have learned that it is a rather accurate picture of bone density. Now, you’re probably thinking that everyone develops wrinkles over time, and that’s true. But there is a difference between ‘life’ wrinkles: from age or sunshine and wrinkles from serious bone decline. So how can you tell? According to a study published in Plastic and Reconstructive Surgery wrinkles are caused by collagen depletion. Remember, both your skin and bones are largely composed of type 2 collagen. Also, wrinkles can be caused by deteriorating facial bones. As you start to lose bone density year after year, that includes your face, too! Which causes the skin to sag and wrinkle.
- Dowager’s Hump. Is a forward curvature of the spine resulting in a stoop. If you have osteoporosis in your spine, it can cause your vertebrae to fracture. This can result in Kyphosis or spinal back hump. In other words, Dowagers humps (Kyphosis) are usually caused by wedge fractures. And yes, you can fracture your back without knowing! For prevention, practice postural exercises regularly.
For a complete list of symptoms, read Osteoporosis Symptoms.
Why Men Are Less Likely To Seek Treatment
The statistics on osteoporosis in men showcase the ugly truth about how older men don’t report their deteriorating bone health to doctors and consequently don’t seek corrective measures. It’s suspected that as many as 25% of all hip fractures occur in men. Of these patients, as many as 20% die in the first year of the fracture. This mortality figure is reported to be higher than for women with the same condition as the complications arising from injury in men are of a more serious nature and reported late so that efficient management becomes difficult. As per the National Osteoporosis Foundation, as many as 80,000 men fracture their hips every year.
In the U.S alone, 2 million men are afflicted with osteoporosis and approximately 12 million men are at risk, yet the chances that they seek consultation from a primary healthcare doctor are slim for their debilitating condition.
In a recent study, scientists found that men who see a primary healthcare physician for low bone mass or fractures/broken bones are more likely to get started on an osteoporosis treatment regimen. However, of the total male population for osteoporosis lesser than 25% of the people visited such healthcare professionals during the study.
The statistics are further corroborated by an analysis done on the insurance claims records of men in the state of Texas. A team from the Medical Branch of University of Texas sifted through the records of more than 17,600 men who were over 65 years of age and had claimed compensation for fracture treatments between the five year period between 2000 and 2005.
To bring further coherence and clarity to the survey, the team went on to classify the resulting data further into demographic, diagnostic, procedural, and clinical parameters. This lead them to another startling discovery: before sustaining a fracture a mere 2.7% of the elderly men were detected with osteoporosis but as many as 17.2% were detected positive following a fracture. This brought out how important it is to have osteoporosis detected on time for men (as well as for women).
Researchers are insistent that visiting a physician and testing for bone density following a fracture incidence may improve the rate of bone medication use among men at high risk for osteoporosis.
How is Osteoporosis Treated in Men?
If you are at risk for osteoporosis but haven’t been diagnosed, get tested.
The gold standard test to see if your bones are healthy and strong is called a DEXA scan.
This is the best test for both men and women. The National Osteoporosis Foundation recommends all men over 70 should get tested. This is much later than the recommendation for women (age 65). And while men don’t need to get tested as early as women if they have not experienced a fracture, they should get tested before age 70. Why? By the time men reach this age, they may already have or be well on their way to developing osteoporosis. Prevention is key. So if you can get tested before age 70, do so.
Once you have your baseline DEXA scan done, you will know where your bone health stands. From there, you will be able to discuss the results with your physician or naturopathic doctor and outline a treatment plan.
The following are common natural treatment options for osteoporosis in men:
- Supplementation: Calcium and vitamin D, plus magnesium, vitamin K2, boron, vitamin C and trace minerals are crucial for bone health. For a plant-based, whole food supplement that has all 13 crucial bone-building minerals, go here.
- Exercise: Regular weight-bearing exercise is key to maintaining and increasing bone strength and density. Sports like soccer, basketball, volleyball, and running are all great ways to stress your bones (in a good way) and build bone strength.
- Lifestyle changes: Cutting out smoking, focusing on better sleep patterns, and eating well are lifestyle changes you can control for healthy bones.
Unfortunately, men already tend to seek help for their bone loss far later than women. And the later they get help, the greater chance of a fracture. Worse, more men die the year after a hip fracture than women. Which is a shocking statistic!
So help the men you care about to avoid unnecessary fractures. Please point them to this important article so they can make an informed decision about their health.
Thanks so much for sharing.





onlinemarketinggurus
March 3, 2016 , 4:50 pmawesome!