Virtually everyone has experienced heartburn after a meal, particularly too large a meal, one eaten too rapidly, or one containing fast food, fried food, fatty meats like bacon or sausage, or a pepperoni-laden pizza. The resulting heartburn, a.k.a., acid reflux can cause slight or close to unbearable sensations.
If you’ve ever wondered what causes reflux, and what you can do to prevent it and treat it naturally, this article is for you. We’ll discuss the most common causes of acid reflux, why acid reflux medications may not be your best option, and effective natural remedies you can try before using a proton pump inhibitor, the most commonly prescribed acid reflux drug with a serious drawback: they promote osteoporosis[1][2].
What is Acid Reflux?
Acid reflux is the backflow of stomach contents into the esophagus that can occur shortly after a meal or when lying down. This causes a burning sensation in the mid-chest. When food is consumed, special cells (called parietal cells) in the lining of your stomach secrete hydrochloric acid, so you can digest it. If the food returns back up your esophagus, so does the stomach acid it contains, producing a burning sensation.
Normally, acid reflux is prevented by the lower esophageal sphincter, a valve that is supposed to close tightly after you swallow food and it moves down the esophagus into your stomach. When the lower esophageal sphincter doesn’t close, for reasons we’ll talk about below, the stomach acid produced to digest your food can flow back up your esophagus.
When this happens all the time, it’s called chronic acid reflux or GERD (gastroesophageal reflux disease) and can damage the lining of the esophagus over time as this sensitive tissue isn’t protected against the acidity of your stomach juices[3].
Common Causes of Acid Reflux or GERD
Some of the most common causes of acid reflux or GERD include:
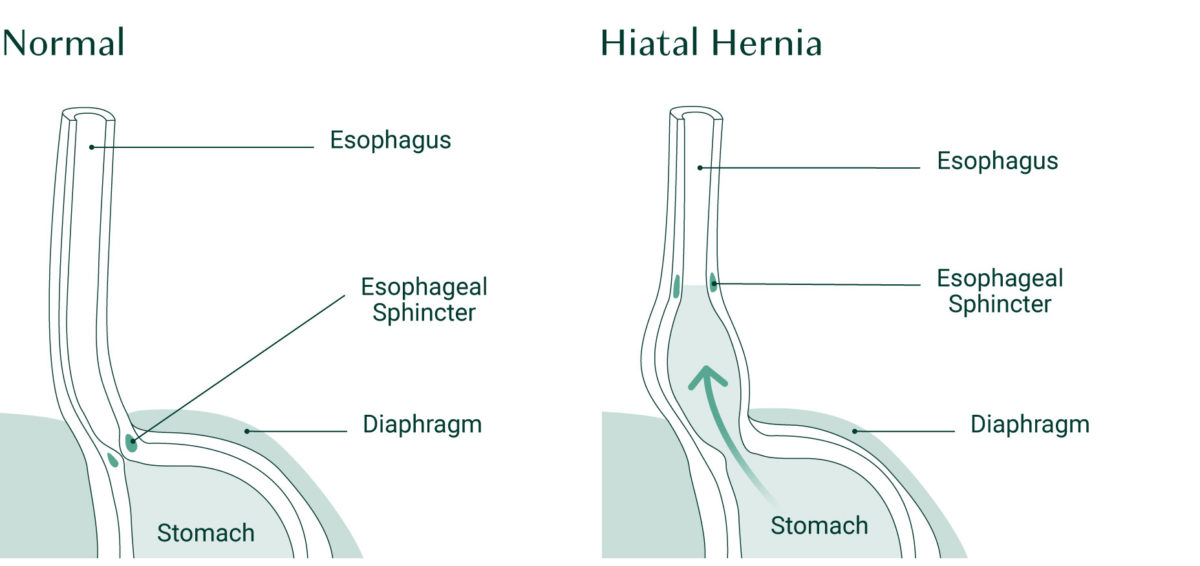
Hiatal Hernia
A hiatal hernia is a condition in which the upper part of your stomach pushes up into the chest cavity through an opening in the diaphragm muscle where the esophagus and stomach join. The diaphragm is a thin wall of muscle that separates your chest cavity from your abdomen. Normally, the diaphragm blocks stomach acid from rising into your esophagus, but when you have a hiatal hernia, the esophageal sphincter’s position is altered, so it doesn’t close completely and can allow food and acid to enter the esophagus, causing heartburn[4].
Hiatal hernias are most commonly caused by increased pressure in the abdominal cavity from physical strain, heavy lifting, straining during a bowel movement, coughing, or vomiting. Risk for hiatal hernias is increased when the connective tissue that is supposed to hold the internal organs and barriers in place is weakened. So having been pregnant and given birth, being overweight or obese[5], or having Ehlers-Danlos Syndrome, a condition that results in overly stretchy connective tissue[6], also increase the risk for the development of a hiatal hernia. If you have a hiatal hernia, surgery is typically recommended. This type of procedure is minimally invasive and may completely fix the problem.
Obesity
Having excess weight around your abdomen can put pressure on your stomach. Ultimately, this may lead to stomach acids moving back up the esophagus, causing heartburn. Some research shows that obese individuals are 2.5 times more likely to experience GERD[7].
Infection with Helicobacter Pylori
Helicobacter pylori (H. pylori) is a bacterial infection that is actually quite common. In fact, it’s estimated that more than 50% of the population have some level of H. Pylori in their stomach. Luckily, at low levels, H. Pylori typically does not cause any issues. However, rising levels can produce a range of symptoms, including heartburn, indigestion, bloating, and belching.
Untreated H. Pylori may even result in more serious issues like chronic gastritis, ulcers, and gastric cancer[3].
The good news is that H. Pylori is easily treated, so ask your doctor to order the urea breath test used to identify the presence of this infection if you have unexplained digestive upset[8][9].
Insufficient Stomach Acid
It may sound funny but having low stomach acid is actually a very common cause of acid reflux. Why? Because we need stomach acid to help break down food in our stomach, and when food isn’t properly digested, it can create gas bubbles that push food and acid back up into your esophagus[10].
Many people find that as they age, their stomach begins producing less acid, and in fact, research shows that 30-50% of postmenopausal women are not producing adequate stomach acid[11][12].
Common Medications
Medications always come with their side effects, and quite a few medications increase the risk for and have been associated with exacerbating GERD. These include: bisphosphonates, long-term use of NSAIDs, oral contraceptives, HRT (particularly estrogen only), nitrates (used for angina, also in conjunction with calcium channel blockers used for high blood pressure and heart diseases), antidepressants (particularly tricyclic antidepressants), benzodiazepines (used as sedatives), and anticholinergics (used for irritable bowel syndrome and overactive bladder)[13].
To pinpoint your cause of acid reflux, discuss your symptoms with your doctor. Don’t self-diagnose or treat it on your own without proper health guidance.
Acid Reflux Medication May Cause Bone Loss
While bone loss medication may cause GERD, it also appears that acid reflux medication may cause bone loss.
One of the most common medications given for acid reflux is proton pump inhibitors (PPIs). In fact, PPIs account for 95% of acid-suppressing drug prescriptions due to their effectiveness[14].
PPIs work by suppressing acid production in your stomach and thereby mitigating GERD. Unfortunately, research shows that long-term use of PPIs increases the risk for osteoporosis due to its negative impact on bone mineral density (BMD)[15].
What’s the connection between PPIs and bone loss?
There are several mechanisms via which PPIs cause bone loss:
#1. PPIs Can Cause Hypergastrinemia
Hypergastrinemia is a condition where the hormone gastrin is higher than normal. Elevated gastrin increases the release of histamine, which impacts bone remodeling by its direct effect on osteoclasts (cells that break down). Specifically, high histamine can increase osteoclast differentiation, resulting in more bone loss than growth[16][17].
#2. PPIs May Promote Hyperparathyroidism
Hypergastrinemia is also related to hyperparathyroidism, which is a condition in which your parathyroid glands release high amounts of parathyroid hormone in the bloodstream. Parathyroid hormone causes your bones to release calcium into the blood, depleting your bones of this vital mineral[18].
#3. PPIs May Cause Hypochlorhydria
Hypochlorhydria is a deficiency in stomach acid. This can happen when PPIs are doing their job a little too well. Having the right amount of stomach acid is crucial for absorbing nutrients, including essential bone-building nutrients like calcium. Therefore, when stomach acid is low, it can result in impaired mineral absorption and poor bone health[19].
Natural Remedies for Acid Reflux
Once you have effectively pinpointed the cause of your acid reflux or GERD, there are a number of things you can try to relieve your symptoms and ultimately heal your digestive system — before turning to acid reflux medications.
Relax
Stress can exacerbate almost every physiological imbalance in your body, including heartburn. When you’re stressed, it directly affects your digestion due to the impact on your parasympathetic nervous system, and research shows a direct correlation between increased stress and increased symptoms of GERD[20].
Finding ways to relax and give your body and mind a break is crucial for overall health. Some tried and true stress-reduction techniques include physical activity, deep breathing, and yoga.

Check out the Ultimate Guide to Yoga for Osteoporosis or How Osteoporosis Affects Mental Wellness for more science-backed, stress-reducing techniques.
Avoid Tight Clothing
Just as extra weight around your abdomen can put pressure on your stomach and cause acid reflux, the same is true for tight clothing. Anything that constricts your stomach can change the way you digest your food, so when you’re experiencing heartburn, bring some awareness to your clothing; if it feels tight around the abdomen, consider trying looser-fitting outfits.
Eat Smaller Portions and Sit Up
The more you eat, the more acid your stomach will need to produce to break down your food. When your stomach is filled with food and acid production is ramped up, it’s a recipe for heartburn. If you tend to eat large meals, try eating smaller portions throughout the day to give your stomach the space it needs to digest your meals with a moderate amount of acid production.
You can also help your digestion by sitting up straight at your meals or going for a short walk after you eat. Whatever you do, don’t lay down – lying down can trigger heartburn as your body has to work against gravity.
Sleep On Your Left Side
While it’s never a good idea to lay down directly after a meal, research shows that when you do go to bed, lying on your left side may be the optimal position for digestion, while sleeping on the right side can aggravate GERD symptoms.
This may be related to the positioning of the lower part of your esophagus (gastroesophageal junction)[21].

Stop Smoking
Smoking is not only detrimental to bone health, but it can also increase acid reflux. When you smoke, it can damage your lower esophageal sphincter (LES), which is responsible for preventing stomach acid from backing up into your esophagus. As your LES muscles become weaker, you may experience more intense bouts of acid reflux[22].
HCL with Betaine
If the cause of your acid reflux is low stomach acid, this can be easily remedied with a supplement containing HCL (hydrochloric acid) with betaine. Everyone’s HCl needs will be different, so finding the right dose takes a little trial and error, but following these guidelines can ensure that you’re getting the right dose for you:
- Begin by taking just one tablet or capsule containing 600 mg of HCl with betaine after consuming a few bites of food at your next meal.
- If this does not aggravate your symptoms, then at every subsequent meal of the same size as the first one, you take one more tablet or capsule. One at the next meal, two at the next meal after that, three at the next meal, and so on. *When you take several tablets or capsules, don’t take them all at once; space them out throughout your meal. Just as your body would normally be producing the hydrochloric acid for you throughout your meal, you want to space out your supplemental hydrochloric acid.
- You can continue to increase the dose until you reach seven tablets or you experience a feeling of warmth in your stomach, whichever occurs first. If you feel any acid reflux from taking your HCl, then it likely means you’ve taken too much, so at the next meal, try backing off by one tablet. The goal is to take just enough HCl to improve your digestion.
Note: A warm feeling in your stomach means you’ve taken too many tablets for that meal. Try the same level of HCl at a similarly sized meal to rule out any factors, such as the type of food you ate. More stomach acid is needed to digest protein than carbohydrates, so a meal containing meat will require more HCl than a vegetarian meal. Try different doses with larger meals until you determine which dose works best, i.e., eliminates your symptoms of indigestion. Obviously, you’ll need smaller doses with smaller meals.
Taking supplemental HCl with betaine can help improve your digestion and your digestive tract’s absorption of nutrients. As your digestive tract receives the nutrients it needs, the parietal cells in your stomach lining, which secrete HCl naturally, will also heal, regaining their ability to produce HCl for you naturally. As this happens, you may find you need less supplemental HCl to assist you.
You may need a bit more HCl when eating bigger or more demanding meals, for instance, if you’re ever going for an “All You Can Eat” buffet or holiday meal. You may also find you need a bit more HCl assistance as you grow older. In most of us, the ability to secrete HCl (at least in the same amounts) drops a little. Try taking an extra capsule and see if your digestion is better or if you get the warm feeling in your stomach. If it’s the latter, you didn’t need extra.
Probiotics for Acid Reflux
Probiotics work to restore and improve the ratio of good-to-bad bacteria in your gut’s microbiome. This can help improve overall digestion and fight off H. Pylori and other pathogens. You can repopulate your system with healthy bacteria by consuming fermented foods along with probiotic supplements. Probiotics have also been shown to benefit brain function and your bones! For more, read our in-depth post on Prebiotics and Probiotics.

Magnesium for Acid Reflux
Magnesium may help lessen acid reflux because it is essential for a well-functioning digestive system. Magnesium relaxes muscles, including those of the intestines, and also prevents hyper-excitability of our nervous system, including the extensive nerve supply to the intestines. Constricted muscles and hyper-excitable nerves can, literally, cramp your digestive style!
However, it’s important to properly balance your intake of magnesium with that of calcium, its partner in many cellular activities. The optimal balance is a calcium: magnesium ratio of 2:1 (or about half as much magnesium as calcium). Consumption of too much magnesium can produce a laxative effect.
Acid Reflux (GERD) Takeaways
Acid reflux is a very common condition. Unfortunately, the drugs used to manage reflux do not address its underlying causes and cause other problems, including mineral insufficiencies that increase your risk for bone loss and set the stage for osteoporosis[23].
Fortunately, you can do much to naturally and safely deal with the causes of reflux and avoid the more dangerous side effects that can occur when it’s left untreated without sacrificing the health of your bones.
Sign up for the AlgaeCal Newsletter to stay informed about the latest research on all things bone health and healthy aging.
FAQs
1. What is acid reflux caused by?
Acid reflux is the backflow of stomach contents into the esophagus that can occur shortly after a meal or when lying down. Several potential causes of acid reflux include hiatal hernia, obesity, infection with H.pylori, insufficient stomach acid, and common medications.
2. How do you relieve acid reflux?
You may find relief from acid reflux by eating smaller portions, avoiding tight clothing, sleeping on your left side, or taking supplements like HCL with betaine. Stress can also exacerbate acid reflux, so try to find ways to reduce stress if you experience heartburn.
3. Is acid reflux serious?
Acid reflux is not life-threatening, but when left untreated, it can cause permanent damage to the esophagus due to ongoing inflammation and irritation. This could turn into esophageal cancer. Acid reflux may also be a symptom of another issue, like a hiatal hernia or H. pylori, so it’s important to get to the root of your reflux.
4. What are the 4 types of acid reflux?
#1 is mild acid reflux, which is the first stage accompanied by mild heartburn. #2 is moderate acid reflux, where symptoms become a bit more frequent and pronounced. #3 is severe acid reflux, characterized by extreme symptoms daily. And #4 is esophageal cancer, which is the result of long-term untreated acid reflux.
5. What does a proton pump inhibitor actually do?
PPIs prevent the proton pump enzymes in the lining of your stomach from making acid. By suppressing acid production in your stomach, they mitigate acid reflux.
References
- Andersen, Bjarne Nesgaard, Per Birger Johansen, and Bo Abrahamsen. “Proton pump inhibitors and osteoporosis.” Current opinion in rheumatology 28.4 (2016): 420-425.
- Ghebre, Yohannes T. “Proton pump inhibitors and osteoporosis: is collagen a direct target?.” Frontiers in endocrinology 11 (2020): 473.
- https://www.mayoclinic.org/diseases-conditions/gerd/diagnosis-treatment/drc-20361959
- https://my.clevelandclinic.org/health/diseases/8098-hiatal-hernia
- Tack, Jan, and John E. Pandolfino. “Pathophysiology of gastroesophageal reflux disease.” Gastroenterology 154.2 (2018): 277-288.
- Nelson, A. D., et al. “Ehlers Danlos syndrome and gastrointestinal manifestations: a 20‐year experience at Mayo Clinic.” Neurogastroenterology & Motility 27.11 (2015): 1657-1666.
- El-Serag, Hashem B., et al. “Obesity is an independent risk factor for GERD symptoms and erosive esophagitis.” Official journal of the American College of Gastroenterology| ACG 100.6 (2005): 1243-1250.
- Alzoubi, Hamed, et al. “The use of 13C-urea breath test for non-invasive diagnosis of Helicobacter pylori infection in comparison to endoscopy and stool antigen test.” Diagnostics 10.7 (2020): 448.
- O’Connor, Anthony. “The urea breath test for the noninvasive detection of Helicobacter pylori.” Helicobacter pylori. New York, NY: Springer US, 2021. 15-20.
- https://my.clevelandclinic.org/health/diseases/23392-hypochlorhydria
- Sipponen, Pentti, and Matti Härkönen. “Hypochlorhydric stomach: a risk condition for calcium malabsorption and osteoporosis?.” Scandinavian journal of gastroenterology 45.2 (2010): 133-138.
- English, Jim. “Gastric Balance: Heartburn and Gastritis Not Always Caused by Excess Acid.” Nutrition Review. Retrieved March 30 (2018): 2022.
- Mungan, Zeynel, and Binnur Pinarbasi Simsek. “Which drugs are risk factors for the development of gastroesophageal reflux disease?.” (2017).
- Thong, Benjamin Ka Seng, Soelaiman Ima-Nirwana, and Kok-Yong Chin. “Proton pump inhibitors and fracture risk: a review of current evidence and mechanisms involved.” International journal of environmental research and public health 16.9 (2019): 1571.
- Chen, C-H., C-L. Lin, and C-H. Kao. “Gastroesophageal reflux disease with proton pump inhibitor use is associated with an increased risk of osteoporosis: a nationwide population-based analysis.” Osteoporosis International 27 (2016): 2117-2126.
- Biosse-Duplan, Martin, et al. “Histamine promotes osteoclastogenesis through the differential expression of histamine receptors on osteoclasts and osteoblasts.” The American journal of pathology 174.4 (2009): 1426-1434.
- Nakamura, Sanae, et al. “Effect of rabeprazole on histamine synthesis in enterochromaffin-like cells of mast cell-deficient (Ws/Ws) rats.” European journal of pharmacology 394.1 (2000): 9-16.
- Gagnemo-Persson, Rebecca, et al. “Growth of the parathyroid glands in omeprazole-treated chickens.” Scandinavian journal of gastroenterology 29.6 (1994): 493-497.
- Thong, Benjamin Ka Seng, Soelaiman Ima-Nirwana, and Kok-Yong Chin. “Proton pump inhibitors and fracture risk: a review of current evidence and mechanisms involved.” International journal of environmental research and public health 16.9 (2019): 1571.
- Naliboff, Bruce D., et al. “The effect of life stress on symptoms of heartburn.” Psychosomatic medicine 66.3 (2004): 426-434.
- Kaltenbach, Tonya, Seth Crockett, and Lauren B. Gerson. “Are lifestyle measures effective in patients with gastroesophageal reflux disease?: an evidence-based approach.” Archives of internal medicine 166.9 (2006): 965-971.
- Parente, F. M. O. S. G., et al. “Cigarette smoking, gastric acid secretion, and serum pepsinogen I concentrations in duodenal ulcer patients.” Gut 26.12 (1985): 1327-1332.
- Koyyada, Arun. “Long-term use of proton pump inhibitors as a risk factor for various adverse manifestations.” Therapies 76.1 (2021): 13-21.






Jan Lemire
March 3, 2018 , 9:28 amI’ve been diagnosed with a hiatal hernia and the doctor said I need to take ranitidine twice a day to stop food from coming up my esophagus, which could help cause cancer. I’m 73 yrs old, still working fulltime, ride my Harley, do 15 mins of chair exercises every day and 10 mins (at least 1/2 mile) on my treadmill at least 4 times a week. Any suggestions?