Dr. William Harris. Dr. Harris is an internationally recognized expert in omega-3 fatty acids and heart disease. The following presentation is a three-part educational series on omega 3 fatty acids – the basics, the benefits and how you can test your levels. This is part two of the three part series, which will cover:
- The HS- Omega 3 Index Test
- The HS- Omega 3 Index and National Media
- What Diseases Can Omega 3’s Reduce Risk For?
- What Percentage Should Your Omega 3 Levels Be At?
- How Much Omega 3s Do You Need and For How Long If Your Levels Are Low?
- Why Red Blood Cells Are Measured Instead of Plasma
For part one of this series, click here.
For part three of this series, click here.
Part Two: The HS-Omega-3 Index from OmegaQuant on Vimeo.
Transcript:
The HS-Omega-3 Index is a measure of the amount of EPA and DHA in red blood cell membranes.
It’s expressed as a percent of the total identified fatty acids. So here is a red cell. Of course, these comprise about half of the blood, the other half is plasma. Each red blood cell has a membrane, like all cells do.
And the membrane, again, can be broken into an outer layer of phospholipids and an inner layer of phospholipids. Each phospholipid has two fatty acids on it: one, two, one, two. In this cartoon, one, two, three fatty acids are EPA or DHA. The others are not. And so we have 3 out of 64 fatty acids here are EPA and DHA. You just do the simple math, 4.6% of the fatty acids in the red cell are omega-3s. Therefore, the HS-Omega-3 Index is 4.6%.
I would note that that HS stands for Harris and Schacky. Professor von Schacky and I came up with the idea in the name of the Omega-3 Index and published it 2004. And so that’s the designation to indicate the assay that we perform in our laboratories is a unique assay. And we think it’s, of course, the best one. But the HS is to indicate an assay that came from either his lab or my lab.
The HS-Omega-3 Index and measuring omega-3 levels has been in the national media.
A variety of reports have come out. The Wall Street Journal reported on it back in October of ’09, “One Fish, Two Fish: Counting Your Omega-3s,” and so this was about omega-3 testing. Dr. Bernadine Healy wrote in U.S. News & World Report in August of ’08 about fish oil in medicine. We’ll look a little bit closer at this one in a moment.
Popular press, Men’s Health back in April of 2010 did a test of the Omega-3 Index. Their editors all got the blood tests and compared it to how much omega-3 they’re eating, and it all made sense. And there was a researcher from the NIH, Dr. Hibbeln, who noted that this is a valid way to monitor your health. And of course, like this paper from the Journal of the American Medical Association, we’ve had several papers published on omega-3 over the years.
Let me go to, specifically, Dr. Healy’s article in the U.S. News & World Report, which was titled “From Fish Oil to Medicine.” Dr. Healy is a past President of the American Heart Association, past Director of the NIH, past Director of the Red Cross, is a cardiologist, and then now is writing commentaries for a variety of magazines.
In her article, she said, and quoting me,
“Based on what we currently know, there is no nutrient more important for decreasing risk for cardiovascular disease and more lacking in our diet than omega-3.”
And then she goes on to say,
“This is no fish story. Raising omega-3s could be as important to public health as lowering cholesterol. Think about that comparison. Reining in our nation’s cholesterol levels over the past 40 years has yielded great benefit to health and longevity. The change was a grassroots effort driven by individuals, both patients motivated by blood tests, and their doctors who help monitor and manage them. The National Cholesterol Education Program even launched a “Know Your Number” campaign. But who knows their level of omega-3s?”
she asks.
And at the end of the article, she concludes with,
“Before long, your personal omega-3 index just could be the new cholesterol, the number you want to brag about at cocktail parties,”
etc. And I agree. I think someday, we will see that everybody’s going to want to know what their omega-3 level is because they can do something about it and they can reduce their risk for disease.
Now, what diseases particularly can the omega-3s reduce risk for?
And I’ll show you some data that really started the story out in the area of primary cardiac arrest. This is a heart attack. It’s also sometimes called sudden cardiac death where the heart actually stops beating, and very quickly, the individual passes away. Obviously a very important disease. About half the people that die of heart disease in a given year die of sudden cardiac death or primary cardiac arrest. 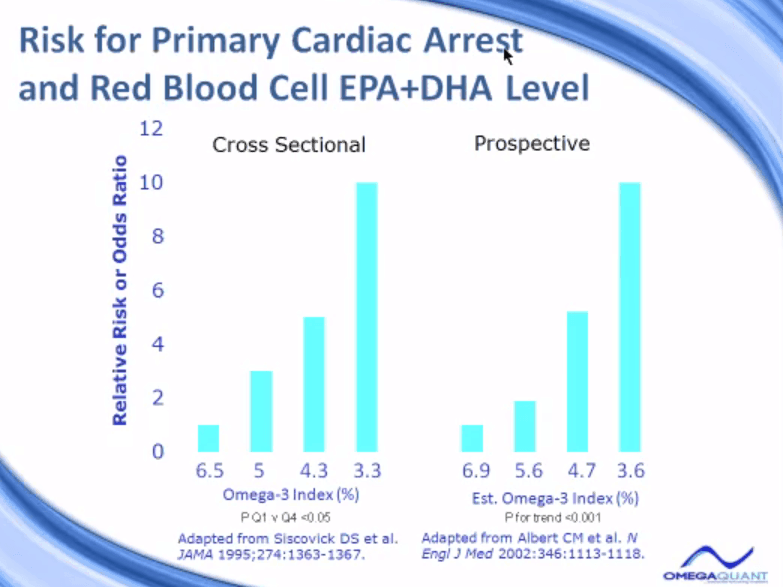
Two different studies have looked at this, and they’ve been designed very differently. They came to the same conclusion though. The people who had the lowest omega-3 levels – down here, 3.3%, 3.6% – had the highest risk for primary cardiac arrest or sudden cardiac death. This study, indicated as a cross-sectional study, meaning that this study, the blood samples that were used in this study were collected all at the same time, and they actually were collected at the time that individuals were having a heart attack.
So the paramedics and ambulance people, when they arrived at the scene, drew a blood sample and stored it from anybody who was having a heart attack on the sidewalk. And that blood samples and analyzer’s compared to other people in the community that were the same age, the same race, the same sex, but not having a heart attack.
And they found that if you look at the quartiles of the omega-3, here’s the group that had the highest omega-3 levels. They were the least at risk. And so we set their risk to one. And then relative to them, those people who had a level only half as much, 3.3%, had a tenfold increase in odds of being actually a case or a sudden cardiac death patient.
In this prospective study done several years later, done in a very different design, in this study, blood samples were collected while individuals were healthy, not when they were having heart attacks, when they were actually healthy and had no evidence of heart disease. The blood samples were then stored, frozen away for many years until a certain number of these individuals actually had a sudden cardiac death experience.
And at that time, which just took 17 years for these events to occur, the investigators in this study went back to the freezer and pulled out the blood samples of those individuals who died of sudden cardiac death. And they also pulled out blood samples, so the individuals who were otherwise matched in every other category, but had not experienced sudden cardiac death. So again, it’s the cases and controls, but this is prospective.
The same story was seen. Those who had the highest omega-3 level will set their risk at one, right here. And then we look, as the omega-3 index goes down, the risk for sudden cardiac death goes up, again, tenfold than those who had the lowest omega-3 levels. So there was a real increase in risk in both settings when the omega-3 index was low.
We looked at a variety of studies, Dr. von Schacky and I, as we wrote this paper back in 2004. We were seeking a value that we could indicate as a healthy target value for the omega-3 index. That’s essential to have if you’re creating a new risk factor. You have to ask, “What is the value that is your target? What’s a good level to aim for?”
So, in so doing, we looked at a variety of studies that have been published, some we’ve looked at, some we’ll look at a little bit later, but we measured or determined what the omega-3 index was in the group that had the greatest benefit in these studies, and it turned out, on average, to be about 8%. From that beginning point, we said, “Well, that looks like a reasonable place to start.” Under 4%’s not good. It looks like on this arrow, the desirable level we are seeing above 8% is the place to be, but that’s certainly subject to more research, but it appears to be holding up, as in studies I’ll show you in a moment.
So the omega-3 index of 8%’s a good level to be at.
Most Americans are down here in the 4% to 5%. In the European Union, the United States, high heart disease risk. In Japan, interestingly, a group or country where a lot of omega-3 is eaten, their omega-3 index is about 9.5% and they have very low heart risk. In fact, in the United States, sudden cardiac death rates are about 20 times higher than they are in Japan. Is that because the omega-3s are very high in the Japanese diet and Japanese blood? I think that plays a role, but we don’t know that for sure.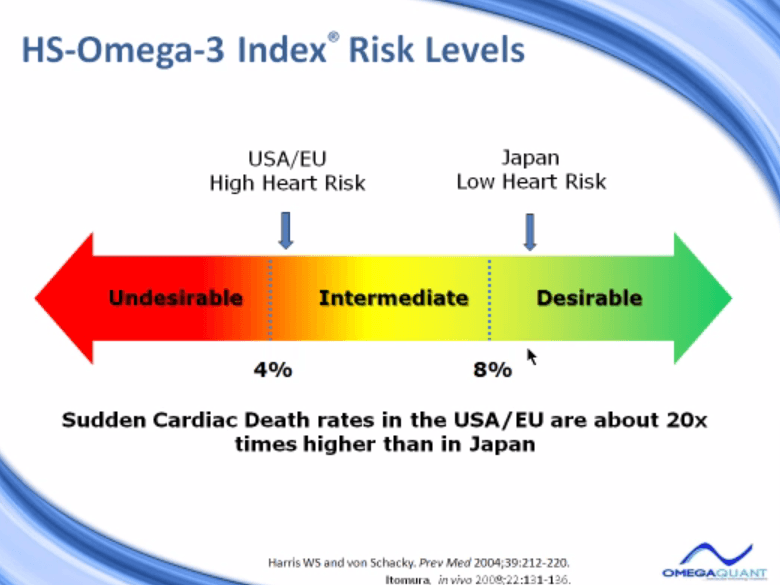
Now, moving from 4% to 8% actually can be done. It’s quite possible to do with dietary change or with taking dietary supplements. So this is a very modifiable risk factor.
But how well does the omega-3 level in a red cell compared to other tissues?
We looked at red blood cell EPA and DHA with human heart myocardial tissues. So this is living human hearts, for people who had heart transplants. Twenty patients were looked at in this study. We measured the red blood cell EPA levels and the omega-3 levels in the heart. We found a very nice correlation, highly statistically significant. And so we know that the omega-3 levels at least relate to or associated with the levels in the heart.
We went on in that study to look at the effects of taking fish oil supplements to raise EPA and DHA levels in these patients. We wondered how it would affect heart omega-3 and red blood cell omega-3. And we found they were affected to the same extent, which means that the red blood cell is a valid surrogate for heart omega-3.
So after six months of 1 gram a day of EPA and DHA in these heart transplant patients, we found that the EPA levels went up about 270% in the heart and about the same amount in the red cell. And they went up about 100% in DHA. So DHA levels went up about 100% in the heart, and about the same in the red blood cell. So again, the omega-3s are a valid marker of cardiac tissue omega-3.
Additional Studies
Other studies we’ve done to look at the validity of the 8% target would include this study, which looked at the relationship between the HS-Omega-3 Index and acute coronary syndromes, that is essentially a fancy way of saying “heart attacks.” We studied 768 cases or individuals who were admitted to the hospital with a bona fide heart attack. And then we recruited 768 controls, individuals who were not coming to the hospital with a heart attack, but who were coming to have blood drawn for some other reason.
And we measured the blood omega-3 levels in both groups. And then we looked at the odds of being a case, of being an acute coronary syndrome patient. And we set that risk at one for those people who had the level of omega-3 under 4%. And then we found that as the omega-3 index went up higher and higher, the fewer and fewer and fewer cases were in these groups. So the odds of being a case were reduced by about 60% or 70% in people who had a high omega-3 index, over 8%.
And these data were calculated and adjusted for all the major risk factors for heart disease, including plasma lipids, LDL and HDL, and a history of heart disease, and age, and gender, diabetes, a variety of things. So this is independent data. The omega-3 is an independent predictor.
Another study we did was done with colleagues at the University of San Francisco. And they were interested in the question – if omega-3 levels predict the rate of cellular aging. And this was done in a study called The Heart & Soul Study. In this study, about 608 patients with stable coronary disease were recruited. Blood samples were drawn at baseline. And five years later, there was no change in their diet, no intervention. They were not told to change anything or given any drugs. They were just following the natural history of the disease.
At baseline, we measured the omega-3 levels in the 608 blood samples, and the investigators there in San Francisco measured what we call telomere length. Telomere length is the length of DNA. It’s a section of DNA at the very tip of each chromosome in every cell. And each time that cell reproduces, the telomere gets a little bit shorter, the length of that tail gets a little shorter. And the more times the cells replicate, the shorter and shorter and shorter the telomere gets, until the point where the cell cannot reproduce anymore. So the length of telomeres, and actually more importantly, the rate of shrinkage, the rate of loss of telomeres is a marker of biological aging.
And so in this study, what they found was that the people who had the lowest omega-3, the lowest quartile of omega-3 levels, had the greatest loss in telomere length over the five years of the study. Those who had the highest omega-3 levels here in quartile four had the least amount of loss. So we would interpret this data to mean that the omega-3 is associated with the rate of cellular aging. A high omega-3, slow aging. A low omega-3, fast aging.
What were the omega-3 index values associated with these quartiles? They’re listed here. The lowest omega-3 quartile was about 3%, on average, omega-3 index. And the omega-3 index at the high end, 8.5%. This, again, supports the idea that a target of 8% is a reasonable target to aim for.
We also asked the question, not only do cells age more quickly with a lower omega-3, we asked, “Do people actually die more quickly?” In the same study, we then measured actual time to death in 982 patients with coronary disease in the Heart & Soul. We just separated the group based on the median omega-3 index, which is 4.6%. So those above and below the median were looked at.
And we found those who had omega-3 index below average died at a faster rate over six years than those who had higher omega-3 levels. And again, this controlled for every other risk factor we were able to find. So it means that the omega-3s are significantly associated with risk for aging and death. That’s an important finding.
Now, let’s move on to the question of how taking omega-3s changes the omega-3 index.
And we’ll look at some studies with Lovaza that we’ve done, a couple here.
First study, we gave 15 healthy volunteers 4 grams a day, 4 capsules a day of Lovaza, which is the indicated dose for triglyceride lowering. But we gave it to normal volunteers for only one month. And then in only 1 month, the omega-3 index went from an average of about 4% up to a little over 7%, which is a very nice increase.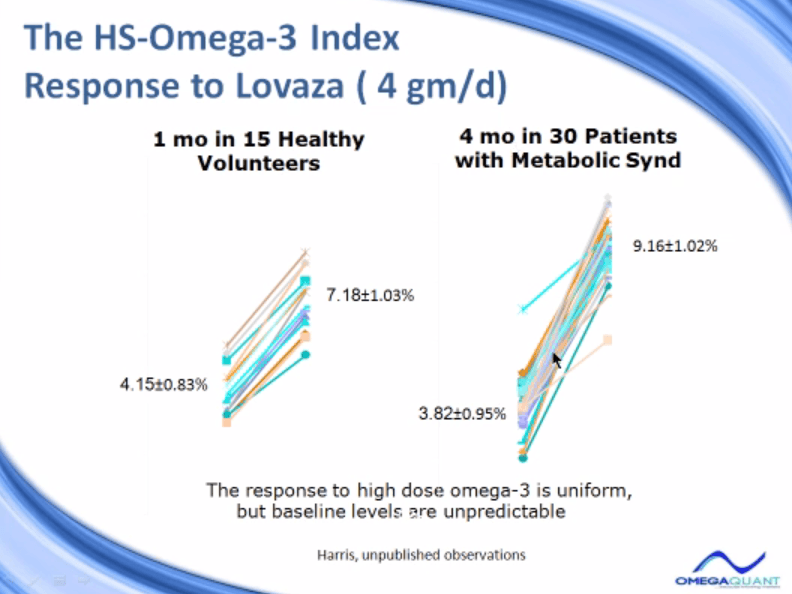
In 30 patients with a metabolic syndrome, we treated them for four months, so much longer treatment period. They began at a lower omega-3 index, which was not surprising. And they ended up, on average, at 9%, which is a very nice increase. So the increase was quite predictable with Lovaza in these trials. What was not predictable was what was the baseline level to begin with. Because the increase was consistent, but the baseline starting was all over the map down here.
And we were interested in digging into this more deeply, so we looked at a variety of studies that we’ve conducted in our lab. Some of these are published, some are not. And we compared the dose here, a little under half a gram a day, 1, 4, 2 grams a day. Different number of weeks of treatment, different kinds of patients, different numbers of patients, and we looked at the beginning and end omega-3. And we were trying to determine how much omega-3 do you need to take for how long to increase your level a certain amount?
So we’ve taken that data that was just in that slide and reduced it to this figure. And in this figure, the line actually is the average for all those studies. And what we’re trying to determine here, with this line, is how much omega-3 does it take to raise your omega-3, to increase your omega-3 index? So to increase it by 4%. This assumes somebody would come in to the office who would have a baseline omega-3 index of about 4%, which is very typical, and would like to achieve the cardio-protective level of 8%. So that’s a 4% increase. So how much omega-3 do you need to do that, and how long do you need to take it?
What we found was that to raise the index by 4% would require about 25 gram-per-day weeks. That’s 25 gram-per-day weeks.
What does that mean? What’s a gram-per-day a week? A 25-gram-per-day weeks is taking 1 gram a day for 25 weeks, or it’s taking 2 grams a day for 12.5 weeks, or 3 grams a day for about 8 weeks. So multiply the grams per day times the number of weeks, and we get this line. And we find out to raise it about 4%, you’d need about 25 gram-per-day weeks.
Twenty-five weeks is about a half a year. So taking about a gram a day for six months should raise your omega-3, on average, by four points. It doesn’t mean you’ll be at 8%. If you started out at a 2% level, maybe it will be at six. But if you started out at 5%, you’ll probably be at 9%. We don’t know what the baseline level is, but the delta is pretty consistent in our studies.
We also looked at, in another study, what is the effect of just simply taking dietary supplements? And this is not Lovaza. This is not a high dose, high-purity omega-3 product, this is simply taking over-the-counter fish oil supplements. In one of our trials, we had 704 normal volunteers, and we basically omega-3 indexed all of them. And we asked them, do they take fish oil pills or not? No fish oil, fish oil. The group that did not take fish oil, only 1% of them had an omega-3 index of over 8%, whereas 75% had index in the red zone, the undesirable zone.
If they were taking fish oil, now, 17% were in the good zone, only 19% in the bad zone. So just the act of taking fish oil supplements… We don’t even know how much they were taking. Typically, people take 1 to 2 capsules a day, which would be 300 to 500 milligrams of omega-3. That, over time, will have a significant impact on the distribution of the omega-3 index and bring 17 times more people into that healthy zone than we see otherwise.
We’ve also looked, over time, what’s the effect, how good a marker is the omega-3 index of omega-3 status in the body, and this was in the Framingham Study, and we looked at the effects of starting fish oil supplementation on the omega-3 index. The way the study was done, and we had about 100 individuals in Framingham for whom we had blood samples in 1999. The same individuals, we had blood samples for in 2006.
And so here, we have about a seven-year period. The question was, if people did not change their omega-3 intake, did the omega-3 index stay stable? Yes, it did. That’s this line right here. No change in intake, no change in index. That indicates this is a good marker of omega-3 exposure.
But how about those people who started taking fish oil between 1999 and 2006? That’s the dotted line started, and there were 41 people who did that, and we found that their index was about 2 units higher, a 41% increase. And we think, from our analysis, about two-thirds of that increase was actually due to taking supplements, and one-third was due to an increase in dietary fish intake. Of course, people who decide to take fish oil or supplements are also the same kind of people that will choose salmon when they go out to eat, instead of a steak. And so this increase reflects a combination of the two.
What is nice, going up two units on the omega-3 index can reduce your risk for sudden cardiac death, based on the studies we’ve already looked at, between 40%, 50%. So this could be very important.
Another reason we like the red blood cell as opposed to plasma is because of its stability in the short term.
The previous study showed long term. Here is a short term biological variability study. We looked at 20 volunteers, we measured blood levels of omega-3, either in the plasma or in red cells, once a week for six weeks. And we told them not to change their diet in any way.
So here was the value, each line is an individual person. And so this is the omega-3 levels in the plasma over six weeks, quite a bit of noise. And here’s the same individuals where the red cell was measured, not the plasma. And all of the noise that’s seen in the plasma is erased by measuring just in the red blood cell.
So the omega-3 index, which is measured in red blood cells, it only has a coefficient, a variation of 4% within person over time. It’s very low compared to 16% in plasma. It is a preferable marker. And the reason is, if you want to know what your omega-3 levels are, you do one blood test and you get the answer.
Up here, if you did a blood test this day and this day in the same person, just one week apart, you’d get a value of 5% here and a 9% here. You wouldn’t know which was true, and you would have to measure multiple times to get an average. With the omega-3 index measured in red cells, you measure it once and you get the right answer. So that’s the best way to have a marker.
Now, we measured the omega-3 index in two different kinds of samples. We measure it in whole blood, liquid blood tubes, the standard blood tubes, and we also measured it in a dried blood spot. And this study was undertaken to see how well our blood spot collection system protected the sample in transit. So we used what we call our QuantCards, these are the dried blood splot cards that we use at OmegaQuant. These are treated with a proprietary mixture of antioxidants, it’s called OxyStop.
And we tested OxyStop-treated QuantCards with, again, some commercially available cards from a company called Fluka, either with BHT – BHT is a chemical antioxidant – or without BHT. And we wondered how over 14 days of storage of a dried blood spot, how stable would the omega-3 index be. We want to see.
What we found here with the OxyStop was very stable levels of omega-3 in the OxyStop-treated cards. But the cards that are treated without BHT or with BHT, both of these cards did not protect as well as the OxyStop-treated QuantCards. So we think this is the really the optimal type card to use for dried blood spot collection.
Once you send in a blood sample to OmegaQuant, we, of course, analyze the omega-3 composition, and the next slide illustrates the result, the kind of paper work we would send back. So this is page one of an OmegaQuant result. Up here on top, you see is the standard demographic: contact information, subject, name, etc. The next line gives really, I think, the most important, single number output of this report, and that’s the HS-Omega-3 Index. And here, it’s 33.2% in this particular individual.
It also has a reference range. Reference range is indicated 0.5% to 10.6%. This is simply the range in which 99% of the population will fall. It doesn’t mean necessarily it’s a healthy range, it just means that’s where the American population is, and the 3.2% certainly falls in that. As we’ve said before, we like to see everybody up over 8%, that would be our desire.
We also, of course, provide the arrow, a visual result, with the desirable results, a target shown. We provide a primary interpretation, which simply is your advice to increase your omega-3 fatty acid intake if your level is well below the 8% target. And finally, some suggestions and discussion that helps people know how to make these changes. Of course, the suggested amount, we suggest here, 3 grams a day, 1 to 3 grams a day will have to be tailored to each individual because there are differences in responses from person to person.
The second page of the report gives far more information, but I think, frankly, perhaps less useful information than the simple one-number omega-3 index. So here, we add up all the omega-3 fatty acids in the dried blood spot, all the omega-6, the monounsaturates – the omega-9, omega-7 – and the saturated fatty acids. And we give you totals, and we give you the standard ranges, the 99% range for each of these.
We also provide the trans fatty acids.
This is a useful marker, I think, because the trans fats are not made in the body, they only get in the body by being eaten. And as in America, we’re trying to reduce the trans fat intake. And so an individual or a physician could follow the changes in trans fats in his or her patient as a function of adopting a more healthy diet. There should be a decrease in the level of trans fats if people are eating better.
We also provide some fatty acid ratios.
Some individuals like to see omega-6, omega-3, and AA to EPA, arachidonic to EPA. We have less confidence in these as being as useful. We prefer, again, the omega-3 index as the primary reporting mechanism for this test.
On the third page of the report, which you can’t see very well here, of course, is simply a table of fish, how much from a high omega-3 fish, EPA and DHA per serving, the sum of the two, down to low DHA and EPA fish. At the very bottom, we have tilapia, mahi-mahi, cod, catfish, some of these fish that have very little omega-3. And then there’s some summary of some dietary supplements, how much omega-3 they have per pill, and we hope that is useful.
So to conclude, the HS-Omega-3 Index section, it’s the most researched, commercially available omega-3 test available. Since 2004, the test has been used or referred to in 55 of our publications, from Dr. von Schacky, myself, or Dr. Yongsoon Park in Korea who also runs this method. But there are currently at least 17 research studies, 12 of them funded by the NIH that are being done with the omega-3 index, as well as 5 pharmaceutical and nutritional companies that are using omega-3 testing in our laboratory to evaluate omega-3 products.




Pamela larkins
January 18, 2017 , 7:36 amInformative- but too much! Should you take and how much. Simple info. But thankyou for the info. Good job.