Hold on tight, because we’re jumping on a rollercoaster ride of bone health discoveries! Today we’re doing a deep dive into the amazing world of omegas.
In our previous post, we unveiled the jaw-dropping power of omega-3 fatty acids. And we shed light on the shady side of omega-6 fatty acids — those sneaky culprits that can foul up your bone formation.
And while that’s crucial to know, there’s so much more to the story! So we’re unraveling the perplexing puzzle of how omegas function and why you need both. You’ll also discover why most people are chowing down on omega-6 like it’s going out of style.
Plus, we’ll reveal the perfect ratio of omega-6 to omega-3 needed to restore the delicate balance of omegas required to transform your bone health. Let’s get into it!
The Ideal Ratio of Omega-3 to Omega-6
It’s believed that during human evolution, our ancestors consumed a diet with a ratio of omega-6 to omega-3 fatty acids of 1:1, equal amounts of both, creating an ideal physiological balance of these two nutrients.
Today, however, studies report that the modern diet (especially the Standard American Diet) contains a ratio closer to 15:1 or even higher [1].
While it would be ideal to go back to our roots and consume a diet with a ratio of 1:1 omega-6 to omega-3, health authorities agree that a balance of 2:1 to 4:1 is more reasonable given our modern food supply [2][3].
Due to the inflammatory nature of omega-6 fats and the anti-inflammatory nature of omega-3s, a healthy intake of omega-3 fats can provide a range of health benefits, impacting nearly every system in your body. And yes, that includes your bones.
How exactly do omega-3s help with bone health? Read on.
Fat Cells or Bones Cells: How Inflammation Determines Your Fate
Inflammation, specifically the state of your omega-6 to omega-3 ratio, is intimately tied to the fate of your bones. When inflammation is low, your bones are allowed to grow healthy and strong, but when inflammation is high, instead of strong bones – you get more fat cells.
It may sound a little strange, but the key player behind the scenes in this drama is a line of stem cells found in your bone marrow called mesenchymal stem cells (MSC). Stem cells, in general, can develop into many different types of cells in your body. MSCs differentiate into a variety of cells, including bone cells, adipose cells (fat cells) in the bone marrow, cartilage cells, and muscle cells [4].
What determines the fate of MSCs? While many factors have an influence, omega-3 and omega-6 fatty acids play a direct role.
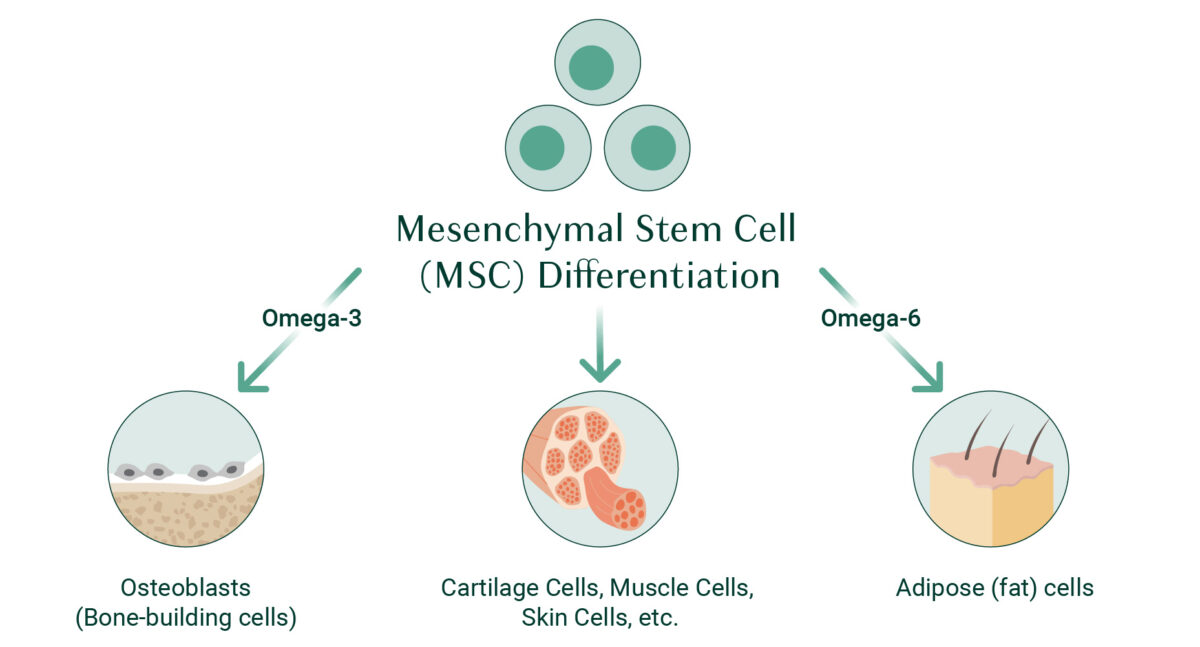
Specifically, signals from omega-6 fats instruct MSCs to differentiate into adipose cells, while signals from omega-3 fats instruct MSCs to turn into osteoblasts (bone-building cells) [5].
To further complicate things, when omega-6 fatty acids are high, they can upregulate the formation of osteoclasts, the cells that break down your bones [6].
Another important factor that can influence the function of MSCs is aging. As we age, stem cells’ ability to differentiate is weakened, and they enter a state known as senescence. When cells become senescent, they can accumulate and potentially promote a variety of age-related diseases – including osteoporosis [7].
Furthermore, research shows that MSCs in older people are more sensitive to inflammation – meaning they’re more likely to develop into adipose cells than osteoblasts [8].
While this may sound bleak, it’s important to remember that the key factor here is inflammation. When inflammation is under control, MSCs are more likely to produce osteoblasts, which means stronger, healthier bones for you.
How Omega-3 and Omega-6 Are Metabolized
While at this point you may feel like omega-6 fats are public enemy number one, the truth is that it really is all about balance when it comes to omega-3s and omega-6s. Bone-building cells are crucial for obvious reasons, but we also need a sufficient amount of bone-resorbing cells to keep bone turnover happening at a healthy rate. Osteoclasts are crucial for clearing out old bone so you can make space for new, healthier growth.
There’s also an important place for inflammation in the overall health of your body. At its core, inflammation is an immune response that’s meant to help you heal. It’s only when inflammation gets out of control that issues arise.
With all of this in mind, let’s look at the metabolism of omega-3s and omega-6s so you can see how things should flow under ideal circumstances and what happens when the ratio of these two nutrients is off balance.
The Shared Enzymes: COX-2 and LOX-5
Omega-3s and omega-6s are both metabolized by the same enzymes; Cyclooxygenase-2 enzyme (COX-2) and 5-lipoxygenase enzyme (5-LOX).
These enzymes produce more inflammatory compounds if your diet is rich in omega-6 fats. If, however, your diet is rich in omega-3s, you’ll get an even balance of pro- and anti-inflammatory compounds, which is ideal for bone health.
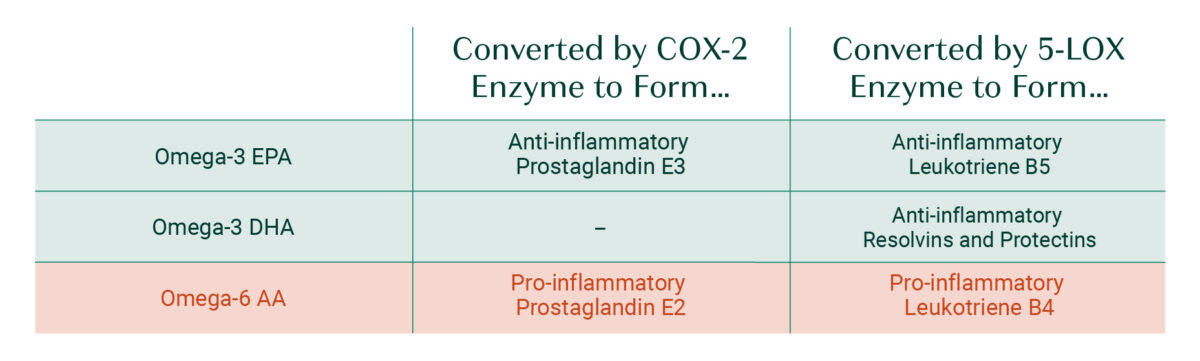
Note: not all omega-6s are converted into pro–inflammatory agents. In particular, gamma-linolenic acid (GLA) can metabolize into anti-inflammatory agents.
Unsurprisingly, research shows that high omega-6 metabolites (prostaglandin E2 and leukotriene B4) are strongly associated with postmenopausal bone loss and obesity [9]. But why are we seeing so many bone health issues today? Our diet has a lot to do with it.
Why Are We Getting Too Much Omega-6?
Put simply; the Standard American Diet is loaded with omega-6 fatty acids. Unlike the diet of our ancestors, our food choices today are processed, packaged, and generally of much lower quality.
To understand why we’re getting too much omega-6 in our diet and find ways to reduce our intake, let’s take a closer look at the main types of omega-6 fatty acids (and where they come from).
LA (Linoleic acid)
Linoleic acid is the most highly consumed polyunsaturated fat in the human diet – meaning it is consumed more than any other omega-3 or omega-6 fatty acid. In fact, some research even suggests that LA accounts for 90% of the omega-6 dietary intake in the US [10][11].
Why are we consuming so much LA these days?
Research shows that over the course of the 20th century, there was a 20-fold increase in the consumption of vegetable oils, which happen to be particularly rich in LA. This was due to a few reasons [12]:
1) Increased availability and low price of these oils.
2) The recommendation of healthcare officials to move away from animal fats in an effort to lower blood cholesterol levels.
3) The increased consumption of processed foods, which tend to use inexpensive fats like vegetable oils.
As our diet has become more ridden with processed foods, our intake of omega-6 fats has naturally increased, and we’re seeing the effects in the number of inflammatory diseases that have taken hold of our society. While many people already deal with inflammatory conditions, according to the NIH, the number of people affiliated with inflammatory diseases is only projected to increase in the next 30 years [13].
To avoid omega-6 overload, use oils with a lower amount of LA (such as olive oil), opt for cooking methods such as steaming, and limit your intake of these LA-abundant foods:

- Vegetable oils (corn, canola, safflower, soybean, sunflower, cottonseed)
- Salad dressings
- Frozen meals
- Baked goods
- Chips, crackers, and popcorn
- Snack and protein bars
- Fried foods
- Coffee creamers
AA (Arachidonic acid)
Arachidonic acid is not only synthesized from the LA that we consume, but is also naturally present in most animal products, including beef, lamb, pork, chicken, duck, turkey, eggs, and fish. While small amounts of AA are vital for several biological systems, including your nervous system, skeletal muscle, and immune system, when you consume too much AA it can instigate unhealthy levels of inflammation [14].
Conventionally raised animals and farmed fish have much higher levels of AA due to the low quality of their feed. In most cases, animal and fish feed is composed of cheap, omega-6 laden ingredients like corn and vegetable oils. This further increases the level of AA in these products – and in your body.
The takeaway? Choose animal products that are either wild, free-range, or organic. And if they are given animal feed, be sure that it’s high-quality.
GLA (Gamma linolenic acid)
GLA is an interesting omega-6 because although it stems from the same inflammatory parent, linoleic acid (LA), GLA has anti-inflammatory benefits. In fact, some research suggests GLA may even protect against DNA damage [15].
Unfortunately, GLA isn’t as abundant as AA and LA in our foods, so we only get this fatty acid in small amounts in our diet. Some GLA-containing foods include hemp seeds, spirulina, oatmeal, flaxseed, evening primrose oil, black currant oil, and borage oil.
Takeaway
All in all, omega-6 fats aren’t inherently bad; we just have a bad habit of overconsuming these types of fats due to their prevalence in today’s food supply.
While reducing processed foods and low-quality animal products will help lower your omega-6 intake, the trick is to ensure you’re getting enough omega-3s as well. In addition to adding wild fish to your diet, a high-quality omega-3 supplement can help you reach a ratio of omegas that is ideal for bone health.
Sign up for the AlgaeCal Newsletter for more insight into bone health and healthy aging.
FAQs
Why is the Omega-3 to 6 ratio important?
Omega-3s are anti-inflammatory, while omega-6s are pro-inflammatory. When in balance, your body is able to carry out health-promoting inflammatory processes without them getting out of control.
What is a good ratio of omega-3 to omega-6?
Ideally, we would be getting a ratio of 1:1 omega-3 to omega-6. That said, it can be challenging to reach that ideal, so health authorities recommend somewhere between 1:2 and 1:4 as an optimal range.
Is omega-6 good or bad for you?
Omega-6 fats in excess can create too much inflammation in your body. That said, we do need omega-6 fats in small amounts for optimal health.
References
- Simopoulos, A. P. (2016). An increase in the omega-6/omega-3 fatty acid ratio increases the risk for obesity. Nutrients, 8(3), 128.
- DiNicolantonio, J. J., & O’Keefe, J. H. (2018). Importance of maintaining a low omega–6/omega–3 ratio for reducing inflammation. Open heart, 5(2), e000946.
- https://www.mountsinai.org/health-library/supplement/omega-6-fatty-acids#
- https://www.mayo.edu/research/labs/bone-injury-repair/research/mesenchymal-stem-cell-biology#
- Levental, K. R., Surma, M. A., Skinkle, A. D., Lorent, J. H., Zhou, Y., Klose, C., … & Levental, I. (2017). ω-3 polyunsaturated fatty acids direct differentiation of the membrane phenotype in mesenchymal stem cells to potentiate osteogenesis. Science advances, 3(11), eaao1193.
- Poulsen, R. C., Wolber, F. M., Moughan, P. J., & Kruger, M. C. (2008). Long chain polyunsaturated fatty acids alter membrane-bound RANK-L expression and osteoprotegerin secretion by MC3T3-E1 osteoblast-like cells. Prostaglandins & other lipid mediators, 85(1-2), 42-48.
- Chen, H., Liu, O., Chen, S., & Zhou, Y. (2022). Aging and mesenchymal stem cells: therapeutic opportunities and challenges in the older group. Gerontology, 68(3), 339-352.
- Laschober, G. T., Brunauer, R., Jamnig, A., Singh, S., Hafen, U., Fehrer, C., … & Lepperdinger, G. (2011). Age-specific changes of mesenchymal stem cells are paralleled by upregulation of CD106 expression as a response to an inflammatory environment. Rejuvenation research, 14(2), 119-131.
- Kruger, M. C., Coetzee, M., Haag, M., & Weiler, H. (2010). Long-chain polyunsaturated fatty acids: selected mechanisms of action on bone. Progress in lipid research, 49(4), 438-449.
- https://lpi.oregonstate.edu/mic/other-nutrients/essential-fatty-acids
- Whelan, J., & Fritsche, K. (2013). Linoleic acid. Advances in nutrition, 4(3), 311-312.
- Jandacek, R. J. (2017, May). Linoleic acid: a nutritional quandary. In Healthcare (Vol. 5, No. 2, p. 25). MDPI.
- Pahwa, R., Goyal, A., & Jialal, I. (2021). Chronic inflammation. StatPearls [Internet].
- https://www.sciencedirect.com/science/article/pii/S2090123217301273
- Rengachar, P., Bhatt, A. N., Polavarapu, S., Veeramani, S., Krishnan, A., Sadananda, M., & Das, U. N. (2022). Gamma-linolenic acid (GLA) protects against ionizing radiation-induced damage: An In vitro and In vivo study. Biomolecules, 12(6), 797.






Dottie Terrano
May 23, 2022 , 4:04 pmThere’s definately a lot to find out about this issue. I love all the points you’ve made.