Dr. William Harris is an internationally recognized expert in omega-3 fatty acids and heart disease. The following presentation is a three-part educational series on omega 3 fatty acids – the basics, the benefits and how you can test your levels. This is part three of the three part series, which will cover:
- Landmark Cardiovascular Trials
- Data on Dementia and Mental Health
For part one of this series, click here.
For part two of this series, click here.
The Benefits: The Science Behind Omega 3 FA’s from OmegaQuant on Vimeo.
Transcript:
Moving now to the third part of this presentation, where we talk about some of the evidence, the benefits of omega-3 increases.
I will look at some landmark cardiovascular trials, and we’ll look at some of the data on dementia and mental health as well.
First to:
Cardiovascular disease.
Epidemiologically, we know that people who eat more omega-3 in their diets have less heart disease and this evidence comes from here, six different trials, five different prospective cohort studies and one cross-sectional study.
Looking at the intake of omega-3 fatty acids in quintiles, 25 milligrams a day up to 566 milligrams a day. And we find that those who are eating the most omega-3 have the lowest rates, roughly about a 40% drop in risk for cardiovascular death than those who are eating the least amounts. So this is a population-based evidence that a higher omega-3 intake is beneficial. There’s also clinical trial evidencek and I’ll talk about three clinical trials that have been successful in showing that omega-3s have benefit.
The first is called the GISSI-Prevenzione trial.
This trial involved over 11,000 patients, post-MI patients who were admitted to the hospital and either given usual care with or without 850 milligrams of EPA and DHA a day. They were given one capsule of the prescription omega-3, which would give you, again, 850 milligrams. This is roughly the amount of omega-3 you would get from three of the standard drug store pills. 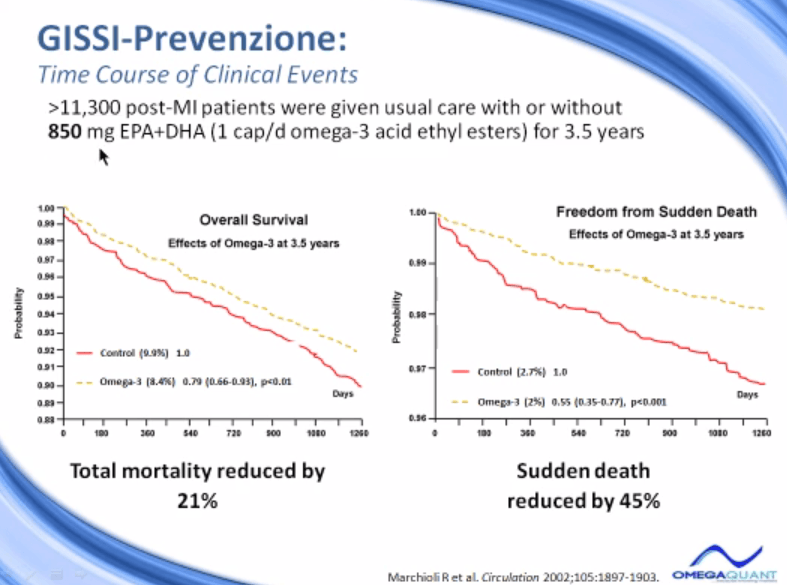
These individuals were followed for three and a half years for overall survival, that means death from any cause, and that was reduced by 21% in the group that got the omega-3. Here’s the rate of death from the control group and the rate of death in the omega-3 group and this difference was a 21% benefit. Another end point was looked at, sudden death.
And interestingly sudden death was reduced by about 45%, a huge difference in sudden death rates in this study suggesting that the omega-3’s actually have anti-arrhythmic effects, not just… And actually the dose used here, one gram a day, they have no lipid-lowering effects whatever. The next study was also a GISSI study and GISSI actually stands for this long acronym. It’s a group of Italian clinics that worked together on trials. This was called the Heart Failure Trial.
And of course patients who have heart failure were recruited, almost 7,000 patients with heart failure, who were on treatments that were appropriate for heart failure patients, a variety of different drugs are used. Half of them were randomized to omega-3, one capsule a day of the prescription omega-3 or one capsule of a placebo. And then they were followed for three and a half, 3.9, let’s say four years for the primary end point, which was a reduction in all-cause mortality.
There was also a sub-randomization and a sub-study buried in this study with rosuvastatin, which is called Crestor in the US. This is one of the more popular statins and they give placebo versus statin to see. And there was no effect on all-cause mortality from giving rosuvastatin in heart failure patients, so I won’t discuss that any further. The results for the omega-3 treatment though can be seen here in this what we call an intention to treat analysis for all-cause mortality total death.
Intention to treat means that everybody who was included in the study, their outcomes are included in the outcome of the end of the study. That is to say even if somebody didn’t take any of the medicine that they were assigned to a group, they never took any, their outcomes, whatever happened to them was included in that group regardless of whether they were compliant or not. This is the most conservative way of actually analyzing these kinds of data.
This was the death rate in the group that got placebo, 29% were dead by the end of the study. And then the fish oil group, for about two years, there was no difference at all, but then the curve started to diverge in the end, 27% of those in the omega-3 group were dead. This is a 9% relative risk reduction and it was statistically significant. As I mentioned, there’s different kinds of ways of analysis. The other way to analyze this data is called the per protocol analysis.
In this way you ask the question,
“Did people who were actually compliant with the medication, who actually took the omega-3s, did they have additional benefit compared to those who took placebo?”
And in this study, there were about 5,000 patients who were considered compliant, who took at least 80% of the omega-3 provided. And now looking at this, there was actually a 14%. As you would expect, a greater benefit in those who actually took the product, 14% drop in risk, highly statistically significant.
So omega-3 treatment can actually reduce risk for total mortality in heart failure patients, even at one gram a day.
The largest omega-3 study that’s ever been done to date is the JELIS study, stands for Japan EPA Lipid Intervention Study. And JELIS is a trial that included almost 19,000 Japanese men and women, mostly women, average age 61, who were randomized to take a statin or statin plus EPA, and the EPA dose was 1.8 grams, followed for five years. 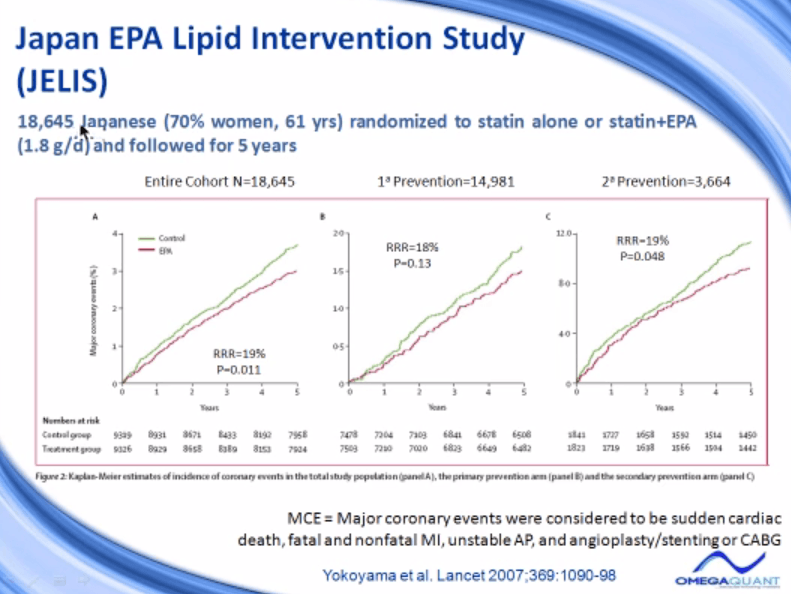
I want to note that everybody in this trial was on statin. They all had high cholesterol levels and therefore they required a statin. Half of them got EPA, 1.8 grams a day. This is about as much EPA as you would get in a full dose four grams a day of Lovaza. So it’s a pretty hefty dose. But again, they did not get any DHA. In Japan, EPA alone is a drug, treated as a drug and that’s what’s being tested in this trial.
The cohort, the entire cohort over 18,000 people. There was a 19% reduction in risk for major coronary events, and that’s the composite end point they used. Major coronary events are defined as sudden cardiac death or fatal, non-fatal MI, or unstable angina or angioplasty/stenting or CABG. So if any of those events happened, that constituted an event, and it countered on this axis here.
The control group had a rate like this. The EPA group had a 19% reduction in risk over five years. They also analyzed just the primary prevention and secondary prevention groups. Primary is people who had no evidence of, no history of heart disease and people with secondary prevention group previously had some heart attack or heart event. And the effect size was the same, the relative risk reduction 18% in this group and that group 19%.
So whether you’ve had a heart disease or not, there’s a similar reduction in risk for major coronary events, at least in this study.
This was not statistically significant. This one was. And the reason in the primary prevention group it was not statistically significant is that there were so few events that actually took place. If you actually look at the scale, at the very end of the study, five years out, less than 2% of the people who had no history of heart disease had had a cardiac event.
If you look over here, the people who had a history of heart disease, here, almost 12% of them had another event. And so the risk was six times higher for people who’ve already got heart disease. This was well-known that people who have already had one heart attack are much more liable to have another one.
Within the JELIS group, there were several studies that were done what we would call sub-studies. When you have almost 19,000 patients, you have a lot of data to work with. One end point they looked at was stroke. Question was, “Did people who got EPA have less strokes, more strokes, no difference?” What they found was if you look at individuals who never had a stroke before, this would be a first stroke, there was no difference in strokes in the EPA or no EPA group. So there was no benefit in that group.
But if you looked at people with high risk for stroke, people who had already had one stroke beforehand, the group that had no EPA had this many strokes and the group that got EPA had a 20% less strokes, a significant reduction.
So there was actually a benefit for stroke in people who had a history of stroke from taking EPA.
Another sub-study that was done in the JELIS was EPA and major adverse cardiac events in the secondary prevention group. This is just those patients who have previous disease. And if they looked at those who had a prior MI only, there was a drop in risk for another event by about 27%, statistically significant. And for those who had had an MI and who’d had had some intervention, like they’d had a heart attack and then they’d have bypass or they’d had a heart attack and then they’d have angioplasty, there was here a 41% drop in risk for another event. Again, the omega-3 is beneficial in secondary prevention as well
Finally we can look at the primary prevention group. This is a group that had no history of heart disease. A particular sub-group of these people, those who had high triglycerides and low HDL were the focus of this study. That’s what we might call the metabolic syndrome. High triglyceride in this study was triglyceride over 150 and low HDL was HDL cholesterol under 40. So any individuals who had, again, in the primary prevention group who had not had heart attack before, but who had a high triglyceride and a low HDL were included in this analysis.
And what they found was that taking EPA reduced the risk of having a major cardiac event in this group by over 50%. Even though the omega-3’s did not reduce triglycerides or raise HDL levels, they still have a tremendous benefit in this particular sub-group at high risk individuals. So those are the three major studies, the two GISSI studies and the JELIS study, that show us in large prospective randomized trials, the benefits of omega-3.
In 2010, there were three studies reported that were negative, or one would actually call them neutral. There was no effect of omega-3. And I want to go over those briefly and talk about what some of the weaknesses of those studies were. The first one is called the OMEGA study. This was done in Germany, a multi-center study, with 3,800 individuals who had suffered an acute myocardial infarction and were randomized to one capsule of Omacor or placebo.
Very similar to the GISSI-Prevenzione study in design, just many, many less patients than the GISSI-Prevenzione study have. They took other drug therapies that were appropriate for modern times. They were followed for cardiac events for one year, and they didn’t find any effect. One year was the problem. They didn’t go long enough. They didn’t have enough events. Sudden cardiac death was not different, total death was not different, and so what was the problem? As I mentioned, the duration was too short.
But what that means, essentially, is that the statistical power of the study was too low. It was under powered. And I’ll quote what they said in the paper then I’ll interpret it. They said, “On the basis of the present results, the anticipated statistical power of 80% was not reached. In an a posteriori calculation, the statistical power was 44% to detect a 45% risk reduction for sudden cardiac death and 19% for a risk reduction of 25%.”
Now, what that means is, if omega-3 treatment in reality reduces risk for sudden cardiac death by 25%, which is a significant reduction in risk if we actually knew that the omega-3’s did reduce risk by that much, then this study would have had one chance in five of actually observing that because there were so few events. So there were four chances out of five that they would come up with a non-significant result, even if there had been a real, in the background, a real effect.
This study cannot conclude that omega-3s did not lower risk for sudden cardiac death. It can only conclude that it was under powered to detect the change. A second study that was published this year was a much lower dose study. This was 4,800 patients with a history of an MI, even up to 10 years ago. They were randomized to EPA and DHA, only 376 milligrams, ALA 1.9 grams, both, or neither.
And in this study, the omega-3 fatty acids were blended into tub margarines, and the margarines were then given to the 4,800 patients and they were asked to use those margarines a certain number of servings a day to get the omega-3. So this was more of a nutritional study than a drug or therapeutic study. They did not find an effect. After 40 months, the fatal coronary heart disease, EPA group versus the non-EPA group, there was actually benefit in the first couple of years, but by the end of the study there was no difference.
The long-chain omega-3 group caught up and there was actually, by almost three years, the same amount of death in both groups. Fatal coronary disease outcome for ALA versus those who were not getting any ALA, no difference at all, so they conclude no effect of treatment. Why? What’s the problem? The problem here is the very low dose of omega-3 that was given.
EPA and DHA recommendations for individuals who have had a heart attack, according to the American Heart Association are around one gram a day.
This is about one-third of that, so I think they were simply under-dosed in this trial. The third study that came out this year that was not successful for showing the benefit of omega-3 was called the SU-FOL-OM3 study, which is a mouthful, but that stands for supplementation with folic acid or omega-3.
Only 2,500 patients with a history of coronary disease in the previous year were randomized to one of four treatment groups, followed for 4.7 years. Here the intake was 600 milligrams a day, that’s better, or they got a B-vitamin cocktail to lower homocysteine. They got both or neither. No effect was shown, reported no effect. What’s the primary problem? Low dose, and I would also say a very small sample size, were not able to detect the effect.
So none of these studies properly addressed the question of the effects of omega-3. I’d like to move this briefly to a couple of studies in the area of dementia and depression, or essentially we’re going above the neck. The heart, of course is below the neck. Above the neck, the omega-3’s also have some benefits. This study looked at… And this is very interesting. This study measured plasma levels of DHA.
This would be not red blood cell, but a measure of plasma. This was well-correlated with red blood cells, and I think the results would imply the same thing would have been seen if they’d measured red cell. They measured the development of dementia in Alzheimer’s disease as a function of the amount of DHA in the plasma. So DHA content of plasma, this is a big word, phosphatidylcholine, that’s a certain lipid in the plasma, it’s a phospholipid, was measured in about 900 subjects who were 76 years of age at the time the blood was taken.
This is from the Framingham Heart Study. And then they looked at the incidence of dementia or Alzheimer’s disease over the next nine years in those 900 patients who were 76 to begin with. What they found was, if you look at the rate of developing Alzheimer’s or dementia over… Now they showed us out almost 13 years. The whole study took that long. The individuals who had the lowest three categories of omega-3 levels, from the 75th percentile down to the first percentile, the lowest omega-3 levels, their rate of developing dementia was at about 15%.
About 15% of them developed it by age 85 to 88. But, interestingly, the group that had the highest omega-3, the highest quartile of omega-3, had about 40% less relative risk, it’s actually 0.53, so almost 50% less risk for developing dementia than those who had lower omega-3 levels. This suggests that maybe in the long term, high omega-3 levels will actually protect against developing dementia. This was not an intervention study.
Nobody was given omega-3 treatment. This was simply looking at the power of prediction of a bio-marker measured at the beginning. Again, here’s an association with a higher blood omega-3 level with lower risk for dementia. Let’s look briefly at depression, another obviously mental disease. There’s been quite a bit of interest in the effects of omega-3 on depression. A variety of trials have been done.
The positive trials, those how found a benefit of omega-3, typically gave EPA alone or EPA in higher concentration than DHA. So these studies were successful. There were a few that were in this category that did not show a benefit, but by and large there’s more effect seen here, compared to down here. Your studies where DHA alone or DHA more than EPA was given. These had been uniformly unsuccessful.
And so we would conclude from at least this quick survey that apparently EPA may be a beneficial omega-3 for depression and not DHA. And we’re just beginning to learn what diseases EPA and DHA alone affect more effectively. Next slide is my second to the last slide. This looks at the omega-3 index in 86 patients who have major depressive disorders, which is MDD, major depressive disorders versus 80 controls.
So they’re asking the question,
“Do people who have depression have lower omega-3 levels than people who don’t have depression?”
That’s a good question. It turns out they did. The control level was about 5% and the people with major depression about 3.9% and was significantly lower. This figure simply gives a distribution of the omega-3 index in the two groups. You just look at this as this is a hill that’s behind this hill. You can see this hill from looking from here.
So this is the level of omega-3 across the distribution from about 8% down to 1% in the depressed patientsm from two and a half to about 10% in the controls. So the omega-3 levels were higher across the board in the individuals who had no depression, again suggesting omega-3’s may have benefit. So finally let’s conclude. Epidemiologic and randomized trials show reduced risk for CHD with EPA and DHA intakes in the neighborhood of one to two grams a day.
Recent trials may have failed because of low doses or short follow-up period of time. Small sample sizes also would add to that. And there is emerging evidence for a support of omega-3 in some role in dementia and depression.
I hope this overview has been helpful to you.



david tinnell
January 5, 2017 , 2:04 pmhey i have a Q about the salmon
do u think farm salmon is or not better then wild salmon
y or y not
im just trying to do reach for my sic class