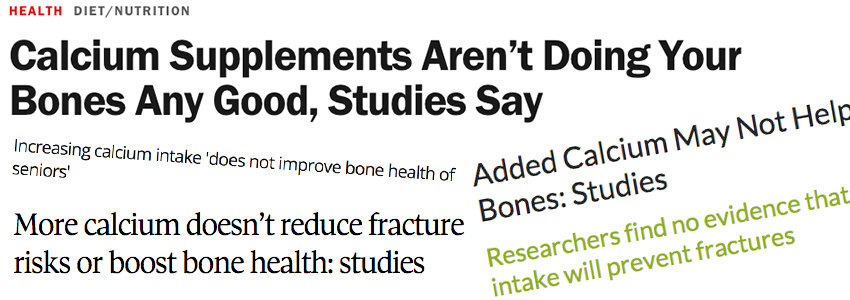
You’ve undoubtedly seen a flurry of media reports on Bolland MJ, et al.’s recently published paper in the British Medical Journal, “Calcium intake and risk of fracture: systematic review.”
Bolland and his co-authors claim that their review of randomized controlled trials and observational studies proves that calcium, whether from foods or supplements, and whether combined with vitamin D or not, has no effect on your risk for fracture. [1]
Balderdash! For so many reasons, which this article will explain in plain English.
I do agree with Bolland et al.’s key point:
Calcium ALONE or with ONLY vitamin D (particularly the inadequate amounts of vitamin D used in the studies Bolland et al. include in their review) is unlikely to prevent fractures.
Nonetheless, this “systematic” review was systematically set up to “show” that calcium, with or without vitamin D, is of no help at all in preventing fractures — and that really bothers me because it’s absolutely not true.
- First, I’m going to share with you the facts. What the studies Bolland et al. choose to include in their review actually show.
- Then we’ll talk about why what Bolland et al. did consider in their choice of studies to review is woefully inadequate, and what this latest attempt to talk us out of getting the calcium we must have for healthy bones actually confirms: our bones need not one, or even two, but the full team of nutrients healthy bones require to remain strong, healthy and fracture-free throughout our lives.
What The Studies Actually Show
I’m quoting directly from their article in the British Medical Journal (I’m just giving the statistics in understandable English, and I’ve added italics to emphasize the real findings and a couple of comments, which I’ve put in […]):
“In 26 randomized controlled trials, calcium supplements reduced the risk of total fracture (20 studies, 58,573 participants; 11% lower risk of any fracture) and vertebral fracture (12 studies, 48,967 participants, 14% lower risk of vertebral fracture), but not hip (13 studies, 56,648 participants, 5% lower risk of hip fracture [Bolland et al considered a 5% lower risk for fracture “nonsignificant”] or forearm fracture (8 studies, 51, 775 participants, 4% lower risk of forearm fracture [again, Bolland et al., consider a 4% lower risk “nonsignificant”].”
Note that calcium supplementation, either calcium alone or with vitamin D, lowered risk of fracture in every single one of these studies. This is what the facts reported in this paper show, but not what you’ll hear in the press reports.
Why Adequate Vitamin D Matters
Furthermore, only one of all the studies Bolland et al. selected to include in their review provided anything even close to a sufficient dose of vitamin D. Adequate vitamin D is required for humans to absorb calcium effectively. The one study that came close to supplying an adequate dose of vitamin D provided 1,600 iu/day, an amount that is just within the range of current Endocrine Society recommendations for healthy adults. The lowest dose of vitamin D now recommended by the Endocrine Society for healthy adults is 1,500 – 2,000 iu/day. 
In all the other studies considered by Bolland et al., dosages of vitamin D ranged from as low as 240 iu/day to 1,200 iu/day. A dose of 240 iu/day is ridiculously inadequate. In a number of the studies included in this review, dosages were 500, 600 or 750 iu/day. The majority of studies used somewhere between 800 – 1,000 iu/day. All the doses of supplemental vitamin D used in the studies included in Bolland et al.’s “systematic review” are inadequate dosages for virtually everyone.
The current Endocrine Society general recommendation for healthy adults whose blood levels of vitamin D are at least 30 ng/mL is 1,500 – 2,000 iu/day. Current research has shown that individuals whose blood levels of 25(OH)D are lower than 30 ng/mL require more than 2,000 iu/day to restore vitamin D adequacy. And the latest research shows that individuals who are obese require 2-3 times more vitamin D than those of “normal” weight. [2]
What were the blood levels of vitamin D in the participants in the studies included by Bolland et al. in their review?
We have no idea.
We have no idea if study participants’ blood levels of 25(OH)D (the form of vitamin D circulating in the blood that is used to evaluate vitamin D status) was even considered important for determining the dose of vitamin D that was given. Although all the doses used would have been inadequate for the “average” healthy person, according to Endocrine Society Guidelines. Participants’ actual blood levels of vitamin D, and therefore how much supplemental vitamin D might have made a significant difference in fracture prevention for them was not considered important enough to evaluate in any of the studies included in Bolland et al.’s review. This, despite the fact that, without adequate blood levels of vitamin D, you will absorb only 10–15% of the calcium you consume, whether from the diet or a calcium supplement.
The latest clinical research on vitamin D has clearly demonstrated that vitamin D supplementation in the range of 1,000–2,000 IU per day is not enough to restore vitamin D to levels able to promote healthy calcium absorption in most individuals with chronic vitamin D deficiency—and this means many of us. According to the Centers for Disease Control more than 30% of children and adults in the U.S. are vitamin D deficient. Other research indicates incidence of chronic vitamin D deficiency is even worse, affecting more than 60% of Canadians and 36% of Americans.[3]
In addition, being significantly overweight or obese can double or even triple our vitamin D requirements. According to the most recent National Health and Nutrition Survey (conducted 2009-2010), more than two-thirds (68.8%) of adults are considered to be overweight or obese. More than one-third (35.7%) of adults are considered to be obese. More than 1 in 20 (6.3%) have extreme obesity. Almost 3 in 4 men (74%) are considered to be overweight or obese.[4]
Given these facts, do you think the inadequate (even for normal weight people) amounts of vitamin D used in the studies included in Bolland et al.’s “systematic review” were going to significantly improve study participants’ calcium absorption? And if you don’t do a good job of absorbing the calcium you consume, how is it going to help prevent fractures?
And let me point out that, despite all of this, calcium alone or with vitamin D still lowered fracture risk in every single one of the randomized controlled trials in Bolland et al.’s review.
The Results Could Have Been Much Better! Why?
Because calcium alone, or even with vitamin D, is not sufficient protection against fractures!
Bolland et al. also did not consider that vitamin D, while absolutely essential for our absorption of calcium, does nothing to regulate what happens to that calcium once inside the body. That is the job of vitamin K2.
Vitamin K2 is the nutrient that we must have to activate the proteins responsible for delivering calcium to our bones (osteocalcin) and preventing calcium from depositing in soft tissues, like our arteries, heart or kidneys.
It’s been well known for more than 15 years now, at least among those who read the peer-reviewed medical literature, that vitamin D not only greatly increases our ability to absorb calcium, but also increases the body’s production of the vitamin K2-dependent proteins, including osteocalcin and matrix Gla protein, which regulate our – healthful – use of calcium. For this reason, vitamin D supplementation actually increases our need for vitamin K2. In addition, it’s also well known that vitamin K2 insufficiency is both widespread and all too common, except in Japan in those individuals who regularly eat the only food that is rich in K2 (in its MK-7 form), natto. (We do get some K2 when healthy bacteria in our gut converts K1 to K2’s short-lived MK-4 form and some K2 in the form of MK-7– MK-10 from certain cheeses and eggs, but the amounts of K2 these foods provide is nowhere near adequate. If you’re not eating natto, your likelihood of K2 insufficiency is astronomically high unless you are taking a supplement that is providing you with at least 100 mcg daily of the MK-7 form of vitamin K2.)
For a very small sampling of the peer-reviewed medical journal articles on the necessity of vitamin K2 for calcium regulation, prevention of cardiovascular disease, kidney diseases and osteoporosis, I have included them in the sources at the end of this article. [5]
Why These Studies Look Good on The Surface – But Are Incomplete and Harmful
So, the apparent “scientific rigor” with which the Bolland et al. “systematic review” was conducted may look good on the surface. But, if you know anything about how calcium use is regulated in a human body, like yours or mine, you will very quickly see that the conclusions drawn by Bolland et al., are based on an incomplete and potentially harmful, understanding of human physiology. What you need to understand is that:
- Our bones require calcium, and we do a very poor job of absorbing calcium without vitamin D. But we need more than just calcium, even if accompanied by adequate amounts of vitamin D!
- Vitamin K2 is essential to prevent heart attacks, strokes and kidney stones in anyone supplementing with calcium, especially if they are also taking vitamin D.
A potentially harmful result of taking calcium along with only vitamin D is that doing this increases our need for K2, as mentioned above, because vitamin D increases our production of not yet activated osteocalcin and matrix Gla protein.
When we take vitamin D, levels of inactive osteocalcin and matrix Gla protein increase in our bloodstream and throughout our cardiovascular system, but they are useless without K2 to activate them. Not only is calcium not delivered to our bones, which become porous, but it is likely to be deposited in the arteries, which become calcified, and also to overload our kidneys, promoting stone formation.
Using calcium healthfully – to build bones, and not calcify arteries or kidneys – requires a team effort.
Your Bones Need a Team Effort. Hut, Hut, Hike!
A football analogy might help here.
- Calcium is the football.
- Vitamin D is the quarterback.
- Vitamin K2, or more specifically the vitamin K dependent proteins, osteocalcin and matrix Gla protein, are the wide receivers.
If plenty of K2-activated receivers are on the field, vitamin D can easily pass the calcium football, either to osteocalcin for a bone-building touchdown or to matrix-Gla protein to prevent the calcium football from ending up in the arteries or kidneys.
When K2 is lacking, our vitamin D quarterback still has to offload the calcium football, but has no K2 receivers ready to accept a pass. Osteocalcin and matrix Gla protein, are sitting on the bench, inactive.
Vitamin D is forced to throw a wild pass. The calcium football flies out and lands somewhere on the field (i.e., in the bloodstream). Drive over. No first down. Or even worse, the pass gets intercepted; our calcium football gets picked up by a player on the opposing (unhealthful use of calcium) team, who scores a goal in … the arteries, the brain, the kidneys? [6]
Past Studies with Similar Results. More of The Same
Several years ago, in 2011, Bolland published other medical journal articles, also in the British Medical Journal, “showing” that calcium supplements with or without vitamin D increase risk of heart attack. [7]
Critiques of these papers immediately appeared in the British Medical Journal and in many other journals. I wrote one of them, entitled “Calcium Supplements Increase Risk of MI—The ‘One Variable’ Emperor is Naked.” The fact that calcium, vitamin D and vitamin K2 are all required for both the healthy absorption and use of calcium was discussed. [8]
The latest Bolland et al., attack on calcium, with or without vitamin D, is just more of the same — ill-informed, unaware of (or refusing to acknowledge) the research – misinformation. It’s a spiffed up version of the Emperor’s Clothes because they added in (an inadequate amount of) vitamin D, but Bolland’s Emperor is still naked! So, it’s time, once again for a reality check, time to again suggest Bolland et al. consider some key facts about how human physiology works — because he certainly didn’t get the message several years ago.
And because Bolland and his co-authors didn’t read the research or chose to ignore reality – i.e., the interactions among calcium, vitamin D and vitamin K2 — a lot of money was wasted to inform us that calcium alone, or with vitamin D, is not sufficient to prevent fracture. Well, of course. We already knew this!
Why Are Researchers Ignoring The Calcium-Vitamin D- Vitamin K2 Connection?
Unfortunately, Bolland’s ignorance of the calcium-vitamin D-vitamin K2 connection is shared by many of his peers. Another study, for which Consumer Reports very recently sent out an alert, claims that calcium supplements (again, calcium ALONE) increase our risk for kidney stones. This study is not published research. It’s an unpublished research report by Lotfus CJ et al., which will be presented at ASN’s Kidney Week conference in November 2015. But it will, I expect, be given lots of press coverage. [9]
As usual, in the “research” that finds calcium supplementation increases risk of unhealthy calcification, Loftus CJ et al. do not even mention vitamin K2. We are told the researchers have “no idea” why taking calcium alone or with vitamin D might promote kidney stones. Here’s a quote: “Though the pathophysiology is unclear, these data suggest patients at risk of stone formation should be cautious of [calcium] supplementation use.”
Gee, I bet YOU have some idea why supplementing with ONLY calcium might not be a good idea.
IF these researchers passed human physiology in medical school and have kept up with the current studies published in the peer-reviewed medical literature on PubMed (which such ill-informed research designs make me question), they should know that K2 is required to prevent calcification in soft tissues, including calcium oxalate kidney stone formation.
Do I sound exasperated, irritated, way beyond annoyed? You bet. I am so tired of the media trumpeting “findings” that are actually incomplete, shabby “science,” particularly because these “findings,” if mistaken for truth, can really harm us.
My hope is that now that you’ve read this, you will not be among those harmed, and you will be on your guard the next time inadequately informed researchers or the media try to put one over on you.
Reality Check
What Bolland et al.’s latest systematic review actually shows, once again, is:
Effective absorption and healthful use of calcium requires both vitamin D3 and vitamin K2.
Sources:
- Bolland MJ, Leung W, Reid IR, et al. Calcium intake and risk of fracture: systematic review BMJ September 2015;351:h4580 doi: 10.1136/bmj.h4580
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30. doi: 10.1210/jc.2011-0385. Epub 2011 Jun 6. PMID: 21646368
- Holick MF, Binkley NC, Bischoff-Ferrari H, et al. Guidelines for preventing & treating vitamin D deficiency & insufficiency revisited. J. Clin. Endocrinol. Metab. 2012, 97, 1153–1158. PMID: 22442274Wacker M, Holick MF. Vitamin D – effects on skeletal and extraskeletal health and the need for supplementation. Nutrients. 2013 Jan 10;5(1):111-48. doi: 10.3390/nu5010111 PMID: 23306192Holick MF. Evidence-based D-bate on health benefits of vitamin D revisited. Dermatoendocrinol. 2012 Apr 1;4(2):183-90. doi: 10.4161/derm.20015. PMID: 22928075
- NHANES data on obesity prevalence, http://www.niddk.nih.gov/health-information/health-statistics/Pages/overweight-obesity-statistics.aspx, accessed 10-26-15Ekwaru JP, Zwicker JD, Holick MF, et al. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One. 2014 Nov 5;9(11):e111265. PMID: 25372709
- Flore R, Ponziani FR, Di Rienzo TA, et al. Something more to say about calcium homeostasis: the role of vitamin K2 in vascular calcification and osteoporosis. Eur Rev Med Pharmacol Sci. 2013 Sep;17(18):2433-40. PMID: 24089220Bunyaratavej N. [Experience of vitamin K2 in Thailand]. Clin Calcium. 2007 Nov;17(11):1752-60. PMID: 17982197Tsugawa N1 Okano T. [Vitamin K and fracture]. Clin Calcium. 2010 Sep;20(9):1334-40. doi: CliCa100913341340. PMID: 20808041Theuwissen E, Magdeleyns EJ, Braam LA, et al. Vitamin K status in healthy volunteers. Food Funct. 2014 Feb;5(2):229-34. doi: 10.1039/c3fo60464k. PMID: 24296867Yamauchi M, Yamaguchi T, Nawata K, et al. Relationships between undercarboxylated osteocalcin and vitamin K intakes, bone turnover, and bone mineral density in healthy women. Clin Nutr. 2010 Dec;29(6):761-5. Epub 2010 Mar 23. PMID: 20332058 Masterjohn C. Vitamin D toxicity redefined: vitamin K and the molecular mechanism. Med Hypotheses. 2007;68(5):1026-34. PMID: 17145139Adams J, Pepping J. Vitamin K in the treatment and prevention of osteoporosis and arterial calcification. Am J Health Syst Pharm. 2005 Aug 1;62(15):1574-81. PMID: 16030366Pizzorno L. Vitamin D and Vitamin K Team Up to Lower CVD Risk: Part II, The Vitamin K Connection to Cardiovascular Health, May 2009, Longevity Medicine Review, access @ http://www.lmreview.com/articles/view/vitamin-d-and-vitamin-k-team-up-to-lower-cvd-risk-part-II/Pizzorno L. Vitamin K: beyond coagulation to uses in bone, vascular and anti-cancer metabolism, IMCJ 2008 Apr; 7(2): 24-30, IMCJ subscriber access at http://www.imjournal.com/index.cfm/fuseaction/archives.display/action/download/id/8350 Pizzorno L. Vitamin K2: Optimal levels essential for the prevention of age-associated chronic disease. Longevity Medicine Review, August 2011, www.lmreview.com.McCann JC, Ames BN. Vitamin K, an example of triage theory: is micronutrient inadequacy linked to diseases of aging? Am J Clin Nutr. 2009 Oct;90(4):889-907. Epub 2009 Aug 19. PMID: 19692494Vermeer C, Theuwissen E. Vitamin K, osteoporosis and degenerative diseases of ageing. Menopause Int. 2011 Mar;17(1):19-23. PMID: 21427421 Gast GCM, de Roos NM, Sluijs I, et al. A high menaquinone intake reduces the incidence of coronary heart disease.Nutr Metab Cardiovasc Dis. 2009 Sep;19(7):504-10. PMID: 19179058 Beulens JWJ, Bots ML, Atsma F, et al. High dietary menaquinone intake is associated with reduced coronary calcification. Atherosclerosis. 2009 Apr;203(2):489-93. PMID: 18722618Tanko LB, Christiansen C, Cox DA, et al. Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res 2005;20:1912e20. PMID: 16234963 Gerber Y, Melton LJ 3rd, Weston SA, et al. Association Between Myocardial Infarction and Fractures: An Emerging Phenomenon. Circulation. 2011 Jun 27. [Epub ahead of print] PMID: 21709062 Vermeer C, Braam L. Role of K vitamins in the regulation of tissue calcification. J Bone Miner Metab. 2001;19(4):201-6. PMID: 11448011
- Wallace RB, Wactawski-Wende J, O’Sullivan MJ, et al. Urinary tract stone occurrence in the Women’s Health Initiative randomized clinical trial of calcium and vitamin D supplements. Am J Clin Nutr. 2011 Apr 27. [Epub ahead of print] PMID: 21525191 Masterjohn C. Vitamin D toxicity redefined: vitamin K and the molecular mechanism. Med Hypotheses. 2007;68(5):1026-34. PMID: 17145139 Adams J, Pepping J. Vitamin K in the treatment and prevention of osteoporosis and arterial calcification. Am J Health Syst Pharm. 2005 Aug 1;62(15):1574-81. PMID: 16030366. Arterioscler Thromb Vasc Biol. 2000 Feb;20(2):317-27. PMID: 10669626 Spronk HM, Soute BA, Schurgers LJ, et al. Tissue-specific utilization of menaquinone-4 results in the prevention of arterial calcification in rats. J Vasc Res. 2003 Nov-Dec;40(6):531-7. PMID: 14654717
- Bolland MJ, Grey A, Avenell A, et al. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011 Apr 19;342:d2040. PMID: 21505219
- Penston J. Claims do not hold water. BMJ. 2011 Jun 7;342:d3543. doi: 10.1136/bmj.d3543. PMID: 21652762Prince RL, Zhu K, Lewis JR. Evidence of harm is unconvincing. BMJ. 2011 Jun 7;342:d3541. doi: 10.1136/bmj.d3541. PMID: 21652761Metcalfe AV, Nordin BE. A reanalysis too far? BMJ. 2011 Jun 7;342:d3538. doi: 10.1136/bmj.d3538. PMID: 21652759Abrahamsen B, Sahota O. Do calcium plus vitamin D supplements increase cardiovascular risk? BMJ. 2011 Apr 19;342:d2080. doi: 10.1136/bmj.d2080. PMID: 21505220
- Loftus CJ, Volovetz J, Chaitoff A, et al. Effects of Calcium and Vitamin D Supplementation on Known Stone Formers. Abstract # FR-PO943, available at http://www.asn-online.org/abstracts


Linda Enger
November 10, 2015 , 6:59 amOf course I , like so many others feel as if (as so often the case with ongoing nutritional changes in “wisdom” ) are again confused and frustrated. Thank you for your comments about the recent study please on calcium supplements.
PLEASE go into detail your defense of the Stontinum aspect of bone supplementation. I have read very conflicting information on this as well. As a ( on and off with my consistency ) consumer of food based bone support , including and especially algae cal plus /strontium boost I have been strongly aware of the different approaches / and formula of Strontium with differing brand products, ( and pricing !) Add to that the negative press I read at times re the consumption of Stontium supplementation I am REALLY even more confused!
here are some links that I am referring to
http://nof.org/faq/599 (from NAtional Osteoporosis Foundation )
thank you for your help.
Linda