Overview of The Management of Osteoporosis in Postmenopausal Women
Osteoporosis and Menopause | Symptoms | Treatment and Prevention | Glucocorticoids and Osteoporosis
Every woman is different. How we age, how our bodies react to changes over time, diet, environment, and stress are just a few of the factors that create the unique circumstances each woman faces over the years.
Even menopause is different in every woman. When does it start, and when does it end? What areas of your body will feel the effects most dramatically, and what areas will hardly feel a thing?
How is Osteoporosis Related to Menopause?
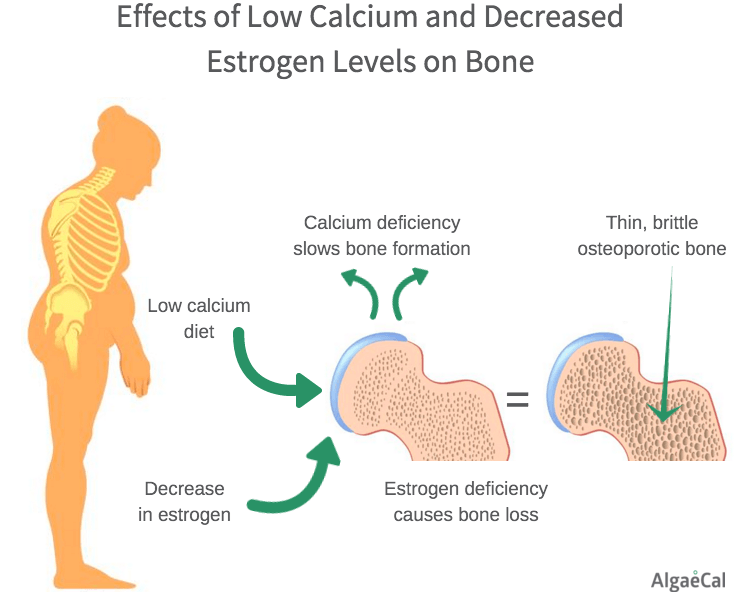
There is a direct relationship between the lack of estrogen during perimenopause and menopause and osteoporosis. Early menopause (before age 40) and any prolonged periods in which hormone levels are low and menstrual periods are absent or infrequent can cause loss of bone mass.
So, Who Gets Osteoporosis?(1)
Important risk factors for postmenopausal osteoporosis include:
- Age. After your body reaches maximum bone density and strength (usually around age 30) bone mass begins to naturally decline as you age
- Gender. Women over 50 have the greatest risk of developing osteoporosis. In fact, women are four times more likely than men to develop osteoporosis. Women’s lighter, thinner bones and longer life spans account for a few the reasons why they are at a higher risk for osteoporosis.
- Ethnicity. Research indicates Caucasian and Asian women are more likely to develop osteoporosis. Additionally, hip fractures are twice as likely to occur in Caucasian women as in African-American women. However, women of color who fracture their hips have a higher mortality rate.
- Bone structure and body weight. Petite and thin women are at greater risk to develop osteoporosis, in part because they have less bone to lose than women with more body weight and larger frames. Similarly, small-boned, thin men are at greater risk than men with larger frames and more body weight.
- Family history. Heredity is one of the most important risk factors for osteoporosis. If your parents or grandparents have had any signs of osteoporosis, such as a fractured hip after a minor fall, you may be at greater risk of developing the disease.
- Prior history of fracture/bone breakage.
- Certain medications. The use of some medications, such as the long term use of steroids (like prednisone) can also increase your risk to develop osteoporosis.
Most cases of osteoporosis occur in postmenopausal women, and the prevalence of the disorder as defined by low BMD increases with age?(2)
Data from the Third National Health and Nutrition Examination Survey indicate:
- 13% to 18% of white American women age 50 or older have menopause and osteoporosis of the hip.
- 37% to 50% have low bone mass (or osteopenia) of the hip
- Osteoporosis rates rise from 4% in women ages 50 to 59 to 52% in women age 80 and older.
- For a white American woman at age 50, the risk of suffering an osteoporotic fracture in her remaining lifetime has been estimated at 40%, with two thirds of the fractures occurring after age 75.
To understand your DEXA results, go here.
Postmenopausal Osteoporosis Symptoms
Postmenopausal Osteoporosis is often called the “silent disease” because bone loss occurs without symptoms.
People may not know that they have osteoporosis until their bones become so weak that a sudden strain, bump, or fall causes a fracture or a vertebra to collapse. Collapsed vertebrae may be first noticed when the person suffers severe back pain, loss of height, or spinal deformities such as stooped posture.
Symptoms generally begin to occur late in the disease when there are not many options to regain the necessary bone density. Below are common symptoms that can indicate osteoporosis:
- Loss of height as a result of weakened spine
- Fractured bones, especially hip bones
- Bone pain and tenderness
- Neck, spine, and lower back pain
- Broken bones, brittle fingernails
- Periodontal disease, tooth loss
Spinal deformities become evident like stooped posture, an outward curve at the top of the spine as a result of developing a vertebral collapse on the back.
Here are some indications that you have postmenopausal osteoporosis:
-
- Low calcium: Calcium deficiency slows bone formation. Menopausal and postmenopausal should increase their calcium intake. You can ensure you are getting enough with a high quality calcium supplement. Symptoms of calcium deficiency include: muscle spasms, memory loss. numbness and tingling in the hands and feet and depression.
- Bone Loss (symptoms and signs above): BMD is an important determinant of fracture risk, especially in women age 65 and older. In general, lower BMDs are associated with a higher risk of fracture. A decrease of 1 SD in BMD represents a 10% to 12% decrease in BMD and an increase in fracture risk by a factor of 1.5 to 2.6, depending on fracture type and measurement. BMD and fracture risk are most closely related when using BMD to predict the fracture risk at that same site. Risks for spine fracture and hip fracture increase 2.3-fold and 2.6-fold, respectively, for each decrease of 1 SD in age-adjusted BMD at spine and hip, respectively.(3)
- Decrease in Estrogen: The increased rate of bone re-sorption immediately after menopause clearly indicates a hormonal influence on bone density in women. The most likely explanation for this increased re-sorption is the drop in ovarian estrogen production that accompanies menopause. Bone loss begins to accelerate approximately 2 to 3 years before the last menses, and this acceleration ends 3 to 4 years after menopause. For an interval of a few years around menopause, women lose 2% of bone annually. Afterward, bone loss slows to about 1% to 1.5% per year.(4)
- Urinary Incontinence: Also known as the loss of bladder control. This can affect your daily routine, but it doesn’t have to. Talk with your doctor about any lifestyle changes or treatment options you may have to ease any discomfort or stop it completely.
Postmenopausal Osteoporosis Treatment & Prevention
Lifestyle approaches alone may not be sufficient to prevent bone loss or reduce fracture risk, but they form a necessary foundation to the prevention or management of osteoporosis.
In some cases, recommended lifestyle approaches may be sufficient. All postmenopausal women, regardless of their bone density or clinical risk factors for osteoporosis, should be encouraged to eat a balanced diet, obtain adequate calcium and vitamin D, participate in appropriate exercise, avoid cigarette smoke and excessive alcohol consumption, and institute fall prevention measures.
These recommendations offer health benefits beyond their effects on the prevention or management of postmenopausal osteoporosis. The recommendations are, in fact, so obvious that their importance may not be appreciated. The success of these approaches is heavily dependent on patient education and motivation to institute them.
- Nutrition: A balanced diet is important for bone development and maintenance, as well as for general health. Some populations, such as women over age 65, edentulous women, women with reduced appetites from any cause, or women who diet frequently or have eating disorders, may not consume adequate vitamins and minerals to maintain optimal bone mass. Older women who lose weight, purposely or not, run the risk of accelerated bone loss and a higher risk of hip fracture.(5)
- Calcium and Vitamin D: Nutritional issues of calcium and vitamin D are perhaps the most important. An adequate intake of both calcium and vitamin D is important for bone health and is recognized as an important component of any osteoporosis regimen.
- Magnesium: Another nutrient, magnesium, is sometimes mentioned as a necessary supplement for the protection of bone health and/ or for absorption of calcium.
- Protein: For women older than age 75, data from the Framingham Osteoporosis Study, a longitudinal cohort study, suggest that adequate protein intake may help minimize bone loss.(6)
- Estrogen Therapy: Systemic estrogen products (estrogen plus progestogen [EPT] for women with a uterus or ET for women without a uterus) are government approved in the United States and Canada for prevention, but not treatment, of postmenopausal osteoporosis.
Globally, approximately 5% of the total population of postmenopausal women take glucocorticoids as a part of their hormone replacement therapy. Though glucocorticoids are very beneficial they come with a slew of side effects such as such as edema of the face and body, palpitations, fatigue, mood swings, vein fragility etc. One of the most dangerous side effects is bone loss. It has been observed that postmenopausal women on hormone therapy lose bone mass rapidly in as early as the first 3-6 months of the hormone therapy. This puts them at an increased risk of developing osteoporosis and of falls and fractures.(7)
In March 2012, the International Osteoporosis Foundation, along with the European Society for Calcified Tissue released new guidelines of the prescription and usage of glucocorticoids with special reference to postmenopausal women. According to Dr. Tobie de Villiers, President of the International Menopause Society (IMS), “The ovaries stop producing estrogen around the time of the menopause, meaning that women find that the risk of bone loss and osteoporosis increases. This is already difficult for many women to cope with, so we need to be especially careful that the medicines which women take for other conditions don’t actually harm women’s bones. Glucocorticoids are important and valuable medicines, but like all medicines they have side effects and their use must be customized and monitored. Women, especially women after their menopause, need to be more aware of the possibility of this serious side-effect. These guidelines are aimed at allowing national organizations to develop effective systems to use glucocorticoids effectively.”(8)
Glucocorticoid Induced Osteoporosis
Glucocorticoids or corticosteroids have direct as well as indirect bearing on the health of bone tissue. Glucocorticoids directly cause the reduction in the manufacture of bone cells osteoblasts thus reducing the rate of bone formation in the body. At another more indirect way, glucocorticoids also alter the body’s processing and channelling of calcium leading to further increase in the rate of bone loss.(9)
Any postmenopausal woman who has been on the hormone replacement therapy for more than 3 months should ask for a bone mineral density test like the Dual energy X-ray absorptiometry (DEXA) to be run to find out her bone health status especially around the hip and spine etc.
It has also been advised that such women who are on glucocorticoids medications for more than 3 months should check their calcium intake. If they are not getting enough through the dietary route, it is recommended they take supplements so that their daily intake of calcium is at least at 1200 mg. Similarly, their Vitamin D intake levels also need to be monitored so as to ensure they are getting between 400 to 1000 IU of vitamin D everyday through either food or supplements. Apart from this, they should be physically active participating in daily walks and moderate weight-bearing exercises which would also go a long way to keeping their weight in check.
Is There a Safe Alternative to Estrogen Therapy?(10)
For those women who cannot take hormone therapy for health reasons or choose not to because of personal reasons, there is a natural alternative…
- Natural Bone Building Supplement. AlgaeCal Plus and Strontium Boost have been shown with clinical trials to increase bone density… naturally, with no side effects. To view the research and results, go here.
How Can I Prevent Postmenopausal Osteoporosis?
There are many ways you can protect your bone health, including:
- Exercise. Exercise on a regular basis. Exercise makes bones and muscles stronger and helps prevent bone loss. It also helps you stay active and mobile. Weight-bearing exercises, done three to four times a week, are best for preventing postmenopausal osteoporosis. Walking, jogging, playing tennis, and dancing are all good weight-bearing exercises.
- Eat foods high in calcium. Getting enough calcium throughout your life helps to build and keep strong bones. The U.S. Recommended Daily Intake (RDI) for calcium for people age 31 to 50 is 1,200 milligrams (mg) a day. People over 50 should get 1,200 to 1,500 mg of calcium each day.
- Vitamin D3. Your body uses vitamin D3 to absorb calcium. Being out in the sun for a total of about 20 minutes every day helps most people’s bodies make enough vitamin D3. You can also get vitamin D from eggs, fatty fish like salmon, cereal and milk fortified with vitamin D. But the best and easiest way to ensure you’re getting enough is from supplements. You should talk to your doctor about getting tested to discover your individual vitamin D needs. For more about vitamin D testing, go here.
- Vitamin K2. Calcium and vitamin D3 are crucial for healthy bones, but a huge part of avoiding bone loss (and cardiovascular and kidney disease) is also adding vitamin K2 into the equation. Vitamin K2 in the form of MK-7 in a dose sufficient to balance D3 is important. Why? It is well known that vitamin D boosts calcium absorption. Less widely known (but just as true) is that Vitamin D also increases our need for vitamin K. So, when you take supplemental vitamin D, you are increasing the amount of calcium available in your body and therefore your need for vitamin K. AlgaeCal was far ahead of the curve in adding vitamin K to its bone health formulation. And now you can see other companies starting to follow suit.
- Other preventive steps. Limit the amount of alcohol you drink, and do not smoke. Smoking causes your body to make less estrogen, which protects the bones. Too much alcohol can damage your bones and increase your risk of falling and breaking a bone.
All women in menopause and osteoporosis should be encouraged to employ lifestyle practices that reduce the risk of bone loss and osteoporotic fractures: maintain a healthy weight, eat a balanced diet, obtain adequate calcium and vitamin D, participate in appropriate exercise, avoid excessive alcohol consumption, not smoking, and use measures to prevent falls.
- Supplement with a plant-based bone mineral supplement. AlgaeCal Plus contains ALL 13 known essential bone supporting minerals, including calcium, magnesium, and boron. Plus the vital vitamins C, D3, and K2. Calcium carbonate and calcium citrate are poorer forms compared to AlgaeCal Plus. Find out why with this clinical study comparing them.
Check out the latest offer from AlgaeCal when you click here.
Sources:
- WebMD.com
- menopause.org/docs/default-document-library/psosteo10.pdf
- Kanis JA, Glu¨er CC, for the Committee of Scientific Advisors, International Osteoporosis Foundation: an update on the diagnosis and assessment of osteoporosis with densitometry. Osteoporos Int 2000; 11:192-202.
- Recker RR, Lappe J, Davies K, Heaney R. Characterization of perimenopausal bone loss: a prospective study. J Bone Miner Res 2000; 15:1965-1973.
- Ensrud KE, Ewing SK, Stone KL, Cauley JA, Bowman PJ, Cummings SR, for the Study of Osteoporotic Fractures Research Group. Intentional and unintentional weight loss increase bone loss and hip fracture risk in older women. J Am Geriatr Soc 2003;51:1740-1747.
- Hannan MT, Tucker KL, Dawson-Hughes B, Cupples LA, Felson DT, Kiel DP. Effect of dietary protein on bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res 2000;15:2504-2512.
- Menopause Clinicians Support New Advice On Steroid Use; Science Daily News; April 2012; http://www.sciencedaily.com/releases/2012/03/120330081737.htm?
- Menopause clinicians support new advice on steroid use; International Menopause Society; April 2012;http://www.imsociety.org/pdf_files/comments_and_press_statements/ims_press_statement_30_03_12.pdf
- Glucocorticoid-Induced Osteoporosis; American College of Rheumatology – Practice Management; April 2012;http://www.rheumatology.org/practice/clinical/patients/diseases_and_conditions/gi-osteoporosis.asp
- Cleveland Clinic.org



Article Comments