“Calcium Needs a Nutrient Symphony: The Key to Bone and Cardiovascular Health” ~ Lara Pizzorno, MDiv, MA, LMT
Contradictory Research Findings Regarding Calcium Supplements
Two contrasting studies made headlines this May (2012): one (Li K, Kaaks R, Linseisen J, et al.) reporting data on 23,980 participants in the EPIC-Heidelberg cohort that suggested calcium supplements might increase risk of heart attacks; the other, (Rejnmark L,Avenell A, Masud T, et al.) a meta-analysis of 13 randomized controlled trials involving 70,528 subjects that found — only if accompanied by supplemental calcium — does vitamin D lower risk of all-cause mortality.
How can we make sense of such seemingly contradictory findings? Are calcium supplements good or bad for us?
An in-depth look at what each of these studies actually investigated and all their findings (not just one statistic taken out of context for an attention-grabbing headline) can help shed light on why the researchers drew such apparently opposite conclusions. More importantly, getting a panoramic, not just tunnel vision view, can help us put the results of both these studies into a context useful to promote our own health — the raison d’être for all research: its practical relevance for improving our health.
An In-Depth Look at the Research
Let’s take a look at the EPIC-Heidelberg study first. What did this study investigate?
Researchers compared the impact of dietary calcium, i.e., calcium consumed from whole foods, like dairy products and leafy greens, to calcium consumed via two types of supplements: (1) supplements providing calcium along with other minerals and vitamins, and (2) supplements providing only calcium (and lots of it, at least 1,000 mg/day), on risk for “cardiovascular events,” e.g., heart attacks and strokes.
Why were they interested in doing so?
Epidemiological studies – also called population studies — look at the causes or influences of health and/or disease in well-defined populations. Such studies have consistently reported that diets providing plenty of calcium-rich foods are associated with lowered risk for high blood pressure, type 2 diabetes and obesity, each of which is known to increase risk for “cardiovascular events.”
In contrast, two recent meta-analyses of clinical trials suggested that calcium supplements might increase a person’s risk of having a heart attack (myocardial infarction). , (Clinical trials involve a much smaller number of people than epidemiological studies. In clinical trials, researchers take two comparable groups of people and give one group an intervention whose effects they want to measure, while giving the other group a placebo. A meta-analysis of clinical trials is a review of the combined results of a number of, hopefully very similar, clinical trials. In real life, the two groups of people compared in a clinical trial may differ in important ways, and meta-analyses are often flawed by combining data from clinical trials that also differ in key ways. The point being: to decide whether the headline you read has any real practical relevance to your health, find out as much as you can about what was actually done.)
Okay, back to the Epic-Heidelberg study (Li K, Kaaks R, Linseisen J, et al.). These researchers decided to use the epidemiological data collected on the Heidelberg cohort, a group of 25,540 Germans aged 35-64 years in 1994-1998 when the study began, to see if they could find any associations between calcium intake from the diet versus calcium from supplements with risk for heart attack, stroke and overall risk of death from cardiovascular disease.
What did the data actually show?
First, they found that dairy foods and beverages (cheese and milk) were the main sources of dietary calcium for this population, providing 39.9% and 28.2% of their daily calcium intake, respectively. When they looked at those using calcium supplements, they found that some took calcium-only supplements, while others took supplements providing not just calcium, but calcium along with other vitamins and minerals.
People with a higher dietary calcium intake were found to also share a number of health-promoting traits including less likelihood of being overweight/obese or smoking, and higher likelihood of being physically active. All of which, as numerous studies have shown, would have lessened their risk for “cardiovascular events.”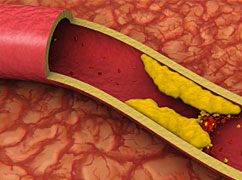
Higher dietary calcium intake also resulted in higher intake of vitamin D, saturated fat and protein. Remember, the primary source of dietary calcium was dairy foods, which are typically fortified with vitamin D, contain saturated fat and are good sources of protein. Higher dietary intake of calcium via dairy foods would also have resulted in higher intake of vitamin K2 since cheeses are a key source of vitamin K2. The researchers, however, did not even consider this or look to see how much K2 those consuming more calcium-rich foods were getting – an omission of major importance in terms of health outcomes discussed below.
Another fact not reported in the headlines: those with the highest dietary calcium intake were also likely to be taking supplements containing calcium (not calcium by itself, but calcium along with other vitamins and minerals).
After an average follow-up time of 11 years, those whose diets supplied the most calcium (an average of 820 mg/day), primarily from dairy foods, were found to have a 30% lower risk for heart attack compared to those whose diets provided the least calcium. As noted above, those with the highest dietary calcium intake were also likely to be consuming more vitamin D, more vitamin K2 and to be taking supplements containing calcium in combination with other minerals and vitamins.
I hope you are beginning to get the drift here – the headlines don’t do justice to the data, do they?
An earlier meta-analysis of other clinical studies conducted in Europe had shown that higher consumption of milk, a major dietary source of calcium in Western countries, was strongly associated with a decreased risk of ischemic stroke. However, the researchers noted, “it is hard to conclude that this inverse association is mainly driven by the calcium content.” I completely agree. Human physiology dictates that calcium alone is not only unlikely to reduce risk for “cardiovascular events,” but can increase risk — more on why next.
In contrast to the beneficial effects of dietary calcium, risk for heart attack was significantly increased among users of calcium-only supplements (specifically, in people taking elemental calcium by itself in doses equal to or greater than 1000 mg/day).
What does this suggest? No silver bullet nutrients exist. Nutrient teamwork is the “sine qua none” of health!
An increased risk for heart attack is just what one would expect from taking calcium in isolation from the other nutrients that regulate how it is used in the body.
You’ve probably already figured this out, so please forgive me for saying it yet again. Calcium in dairy foods is accompanied by a number of other nutrients, e.g., vitamin D and vitamin K (primarily in the form vitamin K2 in cheeses). Taking only calcium in large amounts will cause a calcium overload in the body, resulting in an imbalance in the working relationship between calcium and the other nutrients required for its healthful use.
Fortunately, very few individuals take supplemental calcium by itself, and in large amounts, and also while not consuming foods, such as cheese, omega-3-rich fish and leafy greens, that contain other key nutrients (for example, but not limited to, vitamin D, vitamin K1 and K2) that regulate our body’s use of calcium.
This explains another seemingly contradictory finding noted by the EPIC-Heidelberg researchers: in virtually all the studies looking at calcium supplements and risk for heart attack or stroke, no association has been shown. Making this point, the EPIC-Heidelberg researchers cite:
- A US study of male health professionals, in which no association between calcium supplements and heart attack risk was found.
- A British study of women taking calcium plus vitamin D supplements, again no association was found (even though vitamin D increases our body’s ability to absorb calcium and thus our needs for vitamin K2 to activate the proteins that put calcium into bone and keep it out of arteries, hearts, kidneys, breasts, etc.).
- One study that observed an increased risk of coronary heart disease among women in Finland who took calcium or calcium plus vitamin D supplements, an increased risk likely due in part to insufficient intake of vitamin K2 since vitamin D-rich fish are common fare in Finland. The addition of supplemental vitamin D to an already vitamin D-rich diet would further increase these individuals’ needs for vitamin K2—the reasons for this are discussed below under Vitamin D increases needs for Vitamin K. In addition, not only was the dietary calcium intake in users of calcium supplements in this study significantly less, so they were receiving less of the calcium-regulating nutrients that accompany it in foods, but the women taking calcium supplements were also much more likely to be using conventional hormone replacement therapy (Premarin [pregnant horse estrogens] and progestins [compounds created to mimic a few of progesterone’s actions]) than the women not taking calcium supplements. Conventional HRT is well known to increase risk of venous thromboembolism, cardiovascular disease, strokes and breast cancer.
The EPIC-Heidelberg researchers’ conclusion: “With respect to the associations between calcium supplementation and stroke risk and overall CVD [cardiovascular disease] mortality, this study and all previous observational studies are in agreement on the null associations.” In other words, no associations have been found suggesting calcium supplements increase risk for stroke or death from any type of cardiovascular disease.
So, why does this latest study suggest taking calcium only supplements might increase your risk for a heart attack? After taking a high-dose (>1,000 mg/day) calcium-only supplement, blood levels of calcium can quickly increase, and several studies have observed that high blood levels of calcium can contribute to blood vessel calcification, which increases risk for heart attack.
Interestingly, however, high blood levels of calcium are not seen after eating calcium-rich foods. Why might that be?
First, calcium in food is absorbed more slowly as it has to be digested, which takes time. Supplements, in contrast, are absorbed much more quickly. Even more importantly, calcium-rich foods (and well-balanced supplements) contain the other nutrients — including vitamin D, magnesium, vitamin K1 (leafy greens) and vitamin K2 (cheeses, eggs) — needed to help prevent large amounts of calcium from remaining in your bloodstream and to balance its effects in not just your cardiovascular system, but all your cells, tissues and organs. , , ,
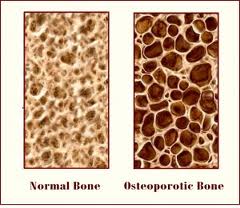
When these nutrients are present, calcium is quickly pulled out of the blood and into cells for its many critical uses in our bodies. In addition to being used to build and maintain our bones and teeth, calcium wears a lot of other “hats,” playing key roles in a variety of critical physiological processes, including helping our blood to clot, so we don’t bleed to death when cut; helping our nerves to send impulses (throughout the body, including the brain), our muscles (including our heart muscle) to contract; and regulating the permeability of our cell membranes, so our cells can allow entry to what they need and send out what they don’t. In sum, every cell in our body requires calcium. When provided with the nutrients required to do so, the human body tightly regulates the amount of calcium in the bloodstream, ensuring just enough is on hand to meet current demands, while delivering the rest where it is needed, including our bones, which also serve as a calcium savings account.
So, what does the Heidelberg-EPIC study really tell us?
Supplemental calcium taken alone in large quantities is not a good idea.
Calcium – when accompanied by the other nutrients needed for its healthful use in the body — as it naturally is in whole foods and in well-balanced supplements – is not only safe, but essential for our health.
Study #2: Rejnmark L, Avenell A, Masud T, et al’s Meta-Analysis: Vitamin D with Calcium Reduces Mortality
Put in this broader context, Rejnmark L, Avenell A, Masud T, et al’s meta-analysis showing supplemental vitamin D lowers risk of all-cause mortality only when accompanied by supplemental calcium — makes sense.
In this study, using pooled data from 13 randomized controlled trials of more than 1,000 participants each (a total of 70,528 participants [86.8% females] with an average age of 70 years), the researchers found that vitamin D alone did not affect mortality, but risk of death was reduced 9% if vitamin D was given with calcium.
They then expanded their meta-analysis to include 24 trials (without size limit) for a total of 88,097 participants. The results were similar: risk of death was reduced 6% with vitamin D plus calcium, but not with vitamin D alone.
In the studies in which vitamin D was used alone, an average of 9.7% of participants died versus less than half that number –4.4% in the studies in which participants took both calcium and vitamin D.
When the analysis of the various studies was restricted to studies in which participants were given both calcium + vitamin D or a placebo, those receiving calcium and vitamin D had a 9% lower risk of death compared to those given placebo.
When analysis of the studies was restricted to those in which only vitamin D (regardless of whether D3 or D2 was used [D3 is more effectively utilized by the body than D2]) or only calcium was used, neither form of vitamin D reduced risk of mortality.
In the studies in which participants were given both calcium and vitamin D, over 3 years of follow-up, risk of death was reduced by 66%!
In an earlier study (2010), the same researchers published results of another meta-analysis showing that vitamin D in doses of 10–20mcg/day (400-800 IU/day) given alone were not effective in fracture prevention, but when given with supplemental calcium, reduced risk for any fracture 8% and risk for hip fracture, specifically, 16%.
Why would calcium + vitamin D be so much more protective against mortality (and fractures) when given together than when either was given individually?
Given the enormous range of health-essential activities in which these two nutrients are involved, the answer to this question could constitute a textbook. Here’s just one example, but one especially apt for bone health: the necessity for adequate supplies of both vitamin D and calcium to prevent excessive production of parathyroid hormone.
High plasma levels of parathyroid hormone (PTH) are known to increase risk of different diseases (including not just osteoporosis, but the full spectrum of cardiovascular diseases and Alzheimer’s disease) and mortality.
Calcium and vitamin D work together to lower PTH levels.
When blood levels of calcium drop too low, the body up-regulates the secretion and activity of parathyroid hormone. Parathyroid hormone increases the production of the most active form of vitamin D (1,25-dihydroxyvitamin D), which helps us absorb more calcium from our intestines (whether from food or supplements), and also increases bone resorption (bone breakdown) to immediately liberate calcium for its many other uses in the body. (Remember above where we talked about calcium wearing a myriad of essential physiological “hats”?)
When we take supplemental vitamin D, we increase our body’s ability to effectively absorb calcium –but only if it’s available from our diet or supplements. If we have calcium in our digestive tract, our blood levels of calcium rise, so PTH levels drop. If we don’t, calcium will be withdrawn from our bones.
In the studies in which only vitamin D was used, the study subjects’ diet may have not provided sufficient calcium for its absorption to affect PTH levels, but when both vitamin D and calcium were provided, PTH levels dropped.
Epidemiological studies have suggested that vitamin D and calcium together affect many different organ systems with widespread effects on our risk for not only osteoporosis and cardiovascular diseases, but type 2 diabetes, obesity, infections, allergies and asthma, autoimmune diseases (e.g., multiple sclerosis), and cancers (in particular, colon and breast cancers).
Vitamin K – the Third Musketeer?
As noted above, along with vitamin D, vitamin K is a top draft pick among nutrients on Team Calcium.
In a three year, double-blind, randomized clinical trial involving 108 postmenopausal women, the carotid arteries of the women given a supplement containing 1000 micrograms/day of vitamin K1 along with 320 IU of vitamin D3, plus magnesium and trace minerals, had more elasticity and ability to respond to changes in blood pressure compared to women who received the mineral supplement alone or the mineral supplement with vitamin D3. The researchers think these beneficial effects were due, in part (remember, it’s a team effort), to vitamin K’s role in reducing calcium deposition in the blood vessel wall.
You may be wondering – why was vitamin K in its form as K1 helpful? Two reasons: (1) If enough vitamin K1 is consumed to more than meet our liver’s needs to be able to produce clotting factors, the rest will be converted to vitamin K2 (in the form of MK-4) and sent out to the rest of the body to activate vitamin-K dependent proteins, like osteocalcin and matrix-Gla protein. (2) While K2 is the form of vitamin K involved in keeping calcium out of our arteries, K1’s potent anti-inflammatory actions are also protective; only after the lining of blood vessels has been damaged by inflammatory insults does the atherosclerotic process begin.
In another study, participants’ levels of osteocalcin (the vitamin K-dependent protein that puts calcium into bone) increased in response to a combination of vitamins D and K, but did not change in response to supplementing with vitamin K alone. Why might that be?
Vitamin D increases our needs for vitamin K
It is well known that vitamin D boosts calcium’s absorption from our intestines and its re-absorption from our kidneys, thus increasing levels of available calcium within the body. Less widely known (but just as true) is that Vitamin D also boosts the expression of the vitamin K-dependent proteins (e.g., osteocalcin and matrix-Gla protein). So, when you take supplemental vitamin D, you are increasing the amount of calcium available in your body and therefore your need for vitamin K, while also increasing levels of the vitamin K-dependent proteins that regulate where that calcium gets deposited (e.g., osteocalcin in bone and matrix Gla-protein in blood vessels). Your body’s physiology is built around an expectation that the full team will turn out to support you in winning the game for your health.
By now, you already have a good idea of what happens when you increase your needs for a robust supply of vitamin K, but do not provide it.
Two studies published April 2011 underscore the importance of an awareness of K2’s role in regulating calcium deposition, and the requirement for K2 sufficient to balance the increased absorption of calcium that occurs when supplemental vitamin D is given. Both studies reported significant increased risk of adverse outcomes in women taking calcium supplements with or without vitamin D – but no vitamin K.
The first study, widely broadcast in the news after it appeared in the British Medical Journal, was a seven year, randomized, placebo-controlled trial of daily supplementation with calcium (1,000 milligrams) and vitamin D (400 IU) in 36,282 postmenopausal women in the U.S. who participated in the Women’s Health Initiative (WHI) study. Supplemental calcium and vitamin D (without any supplemental vitamin K) increased risk of heart attack 24% and the combined risk for heart attack and stroke went up 15%. The second paper, published in the American Journal of Clinical Nutrition analyzed data collected on the same 36,282 postmenopausal women participating in the WHI, this time in relation to whether calcium plus vitamin D supplements increased risk of kidney stone formation. Unsurprisingly, a 17% excess in urinary tract stone incidence was noted in the women taking both supplements.
In the American diet, vitamin K is primarily found as vitamin K1, and its primary sources are leafy greens and canola and soybean oils. Foods providing vitamin K2 (e.g., full fat Emmenthaler and Jarlsberg cheeses, free range eggs and natto) are not consumed daily, or at all, by most Americans. Not only is the standard American diet is sorely lacking in vitamin K-rich leafy greens, but the canola and soy oils used in processed and fast foods are hydrogenated, a process that changes their vitamin K1 into a form in which it can no longer activate the vitamin K-dependent proteins. The end result of all this is that the majority of people in the U.S. are far from consuming sufficient dietary amounts of vitamin K to meet the increased needs for this nutrient when supplemental calcium and vitamin D are taken. The vitamin K status of the women participating in the WHI was not evaluated.
Bet you could you have predicted the negative WHI outcomes.
Unfortunately, neither in the articles reporting these two studies, nor in the press feeding frenzy that occurred after their publication, was vitamin K’s role in regulating calcium even considered. Had it been, these highly adverse outcomes could have easily been avoided.
Warfarin is a drug people with cardiovascular disease are told to take daily to prevent excessive blood clot formation. It works by poisoning an enzyme needed to recycle vitamin K, so causes a functional vitamin K deficiency, and for this reason, is well known to cause calcification of the soft tissues (blood vessels, heart, kidneys). Warfarin is also well known to be much more toxic when taken with vitamin D. Vitamin K alone has been shown to fully reverse the calcification caused by warfarin. 22
You may now be wondering, WHY did the Rejnmark L, Avenell A, Masud T, et al’s meta-analysis discussed above find a 66% reduction over three years of follow-up in the studies in which participants were given both calcium and vitamin D?
A number of the studies used in Rejnmark L, Avenell A, Masud T, et al’s meta-analysis were conducted in countries – Sweden, Norway, Denmark – where the diet is, in general, much higher in vitamin K than in the U.S./Canada. Cheeses supplying vitamin K2 are very frequently consumed in these countries, consumption of leafy greens rich in vitamin K1 (some of which our bodies convert to vitamin K2 once our needs for vitamin K1 have been met) is also significantly higher than in the US/Canada, and fewer processed and fast foods are consumed.
Bottom line: When vitamin K is on your health team, vitamin D and calcium are cardio- and bone-protective.
Vitamin K1 (which you will be getting if you eat plenty of leafy greens like romaine lettuce, collards, Swiss chard, kale, broccoli, parsley, etc.) is sent from your intestines via the portal vein to your liver where its first job is to activate the clotting factors that prevent us from bleeding out from even the tiniest cut. Vitamin K1 is so essential for our survival that our bodies have a special system to recycle it, so we can keep it around longer. Warfarin very effectively shuts down this system, so clotting factors cannot form from vitamin K1. This is why (as mentioned above) people who are taking warfarin are at greatly increased risk of calcifying their arteries and kidneys.
Vitamin K2 has nothing to do with clotting factors. It is not in leafy greens, but is found in tiny amounts in eggs and cheeses (Emmenthaler and Jarlsberg have the most) and in the greatest concentration in the fermented soy bean product called natto. Vitamin K2 activates the proteins that regulate what happens to calcium that you have consumed (whether from food or supplements). It does so by activating the protein responsible for putting calcium into bone (called osteocalcin) and the protein responsible for keeping it out of arteries, kidneys, etc. (called matrix Gla protein). If you do not have enough vitamin K2 on board, and you eat calcium-rich foods or take a calcium supplement, especially if you are taking vitamin D, which significantly increases your body’s ability to absorb calcium and also boosts our body’s production of osteocalcin and matrix Gla protein for vitamin K2 to activate so that calcium can be safely used, then you are going to increase your risk for stroke or heart attack.
The foods in the Western diet that deliver vitamin K2– dairy, eggs and meat – are concentrated sources of cholesterol, saturated fat, and calories, so consuming these foods in amounts large enough to supply optimal amounts of vitamin K2 could promote cardiovascular disease. For this reason, taking a vitamin K2 supplement is advisable to ensure you can activate sufficient levels of the vitamin K-dependent proteins required to help prevent not just osteoporosis and cardiovascular disease, but an increasingly long list of aging-associated diseases, including kidney disease, type 2 diabetes and Alzheimer’s disease, now recognized to be related to vitamin K2 insufficiency. (If you would like to learn more about this, I discuss this research in a free-access review of vitamin K2 written for medical professionals that is available at Longevity Medicine Review.)
CONCLUSION
I hope this helps clear up some of the confusion around taking calcium supplements. It distresses me greatly to think people may stop taking the supplemental calcium and vitamin D we need for healthy bones because of the truncated and misleading way in which research findings are often reported. It is extremely important to recognize that nutrients do not work alone within our bodies! It’s absolutely a team effort—a key reason why AlgaeCal Plus, which delivers calcium in the naturally-balanced matrix of trace minerals used by the sea-algae to create its bony structure, and also provides magnesium, vitamin D3 and vitamin K2 (as MK-7) is more effective in building bone than other forms of supplemental calcium. When team players are missing, our metabolism is very likely to drop the proverbial ball. When Team Calcium is fully present, our bodies will do what we are pre-programmed from birth to do — be gloriously healthy.
References
- Li K, Kaaks R, Linseisen J, et al. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart. 2012 Jun;98(12):920-5. PMID: 22626900
- Rejnmark L, Avenell A, Masud T, et al. Vitamin D with Calcium Reduces Mortality: Patient Level Pooled Analysis of 70,528 Patients from Eight Major Vitamin D Trials. J Clin Endocrinol Metab. 2012 May 17. [Epub ahead of print] PMID: 22605432
- Bolland MJ, Grey A, Avenell A, et al., Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011 Apr 19;342:d2040. doi: 10.1136/bmj.d2040. PMID: 21505219
- Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010 Jul 29;341:c3691. doi: 10.1136/bmj.c3691. PMID: 20671013
- Elwood PC, Pickering JE, Hughes J, et al. Milk drinking, ischaemic heart disease and ischaemic stroke II. Evidence from cohort studies. Eur J Clin Nutr. 2004 May;58(5):718-24. Review. PMID: 15116074
- Al-Delaimy WK, Rimm E, Willett WC, et al. A prospective study of calcium intake from diet and supplements and risk of ischemic heart disease among men. Am J Clin Nutr. 2003 Apr;77(4):814-8. PMID: 12663277
- Shah SM, Carey IM, Harris T, et al. Calcium supplementation, cardiovascular disease and mortality in older women. Pharmacoepidemiol Drug Saf. 2010 Jan;19(1):59-64. PMID: 19757413
- Pentti K, Tuppurainen MT, Honkanen R, et al. Use of calcium supplements and the risk of coronary heart disease in 52-62-year-old women: The Kuopio Osteoporosis Risk Factor and Prevention Study. Maturitas. 2009 May 20;63(1):73-8. Epub 2009 Apr 24. PMID: 19394167
- Modena MG, Sismondi P, Mueck AO, et al. New evidence regarding hormone replacement therapies is urgently required transdermal postmenopausal hormone therapy differs from oral hormone therapy in risks and benefits. Maturitas. 2005 Sep 16;52(1):1-10. PMID: 15963666
- Pizzorno L. Vitamin K2: Essential for the Prevention of Age-Associated Chronic Disease, Longevity Medicine Review, Aug 2011; www.lmreivew.com
- Al-Delaimy WK, Rimm EB, Willett WC, et al. Magnesium intake and risk of coronary heart disease among men. J Am Coll Nutr. 2004 Feb;23(1):63-70. PMID: 14963055
- Mathers TW, Beckstrand RL. Oral magnesium supplementation in adults with coronary heart disease or coronary heart disease risk. J Am Acad Nurse Pract. 2009 Dec;21(12):651-7. PMID: 19958415
- Rosanoff A, Weaver CM, Rude RK. Suboptimal magnesium status in the United States: are the health consequences underestimated? Nutr Rev. 2012 Mar;70(3):153-64. doi: 10.1111/j.1753-4887.2011.00465.x. Epub 2012 Feb 15. PMID: 22364157
- Rejnmark L, Avenell A, Masud T, et al. Vitamin D with Calcium Reduces Mortality: Patient Level Pooled Analysis of 70,528 Patients from Eight Major Vitamin D Trials. J Clin Endocrinol Metab. 2012 May 17. [Epub ahead of print] PMID: 22605432
- DIPART (Vitamin D Individual Patient Analysis of Randomized Trials) Group. Patient level pooled analysis of 68 500 patients from seven major vitamin D fracture trials in US and Europe. BMJ. 2010 Jan 12;340:b5463. doi: 10.1136/bmj.b5463. PMID: 20068257
- Hagström E, Hellman P, Larsson TE, et al. 2009 Plasma parathyroid hormone and the risk of cardiovascular mortality in the community. Circulation. 2009 Jun 2;119(21):2765-71. Epub 2009 May 18. PMID: 19451355
- Chen JS, Sambrook PN, March L, et al. 2008 Hypovitaminosis D and parathyroid hormone response in the elderly: effects on bone turnover and mortality. Clin Endocrinol (Oxf). 2008 Feb;68(2):290-8. Epub 2007 Sep 14. PMID: 17854393
- Braverman ER, Chen TJ, Chen AL, et al. Age-related increases in parathyroid hormone may be antecedent to both osteoporosis and dementia. BMC Endocr Disord. 2009 Oct 13;9:21. PMID: 19825157
- Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011 Jan;86(1):50-60. PMID: 21193656
- Braam LA, Hoeks AP, Brouns F, et al. Beneficial effects of vitamins D and K on the elastic properties of the vessel wall in postmenopausal women: a follow-up study. Thromb Haemost. 2004 Feb;91(2):373-80. PMID: 14961167
- Douglas AS, Robins SP, Hutchison JD, et al. Carboxylation of osteocalcin in post-menopausal osteoporotic women following vitamin K and D supplementation. Bone. 1995 Jul;17(1):15-20. PMID: 7577153 as cited in Gundberg CM, Lian JB, Booth SL. Vitamin K-dependent carboxylation of osteocalcin: friend or foe? Adv Nutr. 2012 Mar 1;3(2):149-57. doi: 10.3945/an.112.001834. PMID: 22516722
- Masterjohn C. Vitamin D toxicity redefined: vitamin K and the molecular mechanism. Med Hypotheses. 2007;68(5):1026-34. PMID: 17145139
- Pizzorno L. Vitamin K2: Essential for the Prevention of Age-Associated Chronic Disease, Longevity Medicine Review, Aug 2011; www.lmreivew.com



Angela
May 6, 2023 , 6:08 pmThank you for sharing info on calcium, vitamin k, vitamin D and thank you for breaking some of the myths that are floating out there