Bone fractures, commonly known as broken bones, come in various forms and stem from numerous causes. Maybe you took a tumble or got hurt playing sports, or perhaps running long distance has led to a stress fracture. Additionally, certain health conditions, such as osteoporosis, can weaken bones and make them more susceptible to breaks even from minor incidents.
When you break a bone, the goal is to heal up as fast and safely as possible. Kids usually bounce back pretty quickly from fractures, but for adults, and especially older folks, it can take a bit longer. And the longer it takes to heal, the more you have to watch out for other problems that might pop up.Here’s some good news, though: there are lots of things you can do to help your bones heal faster, which we’ll dive into later in this article. Plus, we’ll talk about osteoporosis, a condition that makes bones more fragile and prone to breaking, and what you can do about it to keep your bones as strong as possible.
Osteoporosis and Bone Fractures
Bone conditions like osteopenia and osteoporosis significantly increase your chances of breaking a bone. That’s because these conditions make your bones less dense and more fragile, so they’re easier to break.4
If you have osteoporosis, you’re more likely to break bones in places like your spine, hip, wrist, upper arm, and pelvis. But really, when your bones are weak, a fracture could happen just about anywhere in your body.
Here’s a sobering fact: after the age of 50, about half of all women will have a fracture related to osteoporosis at some point.5
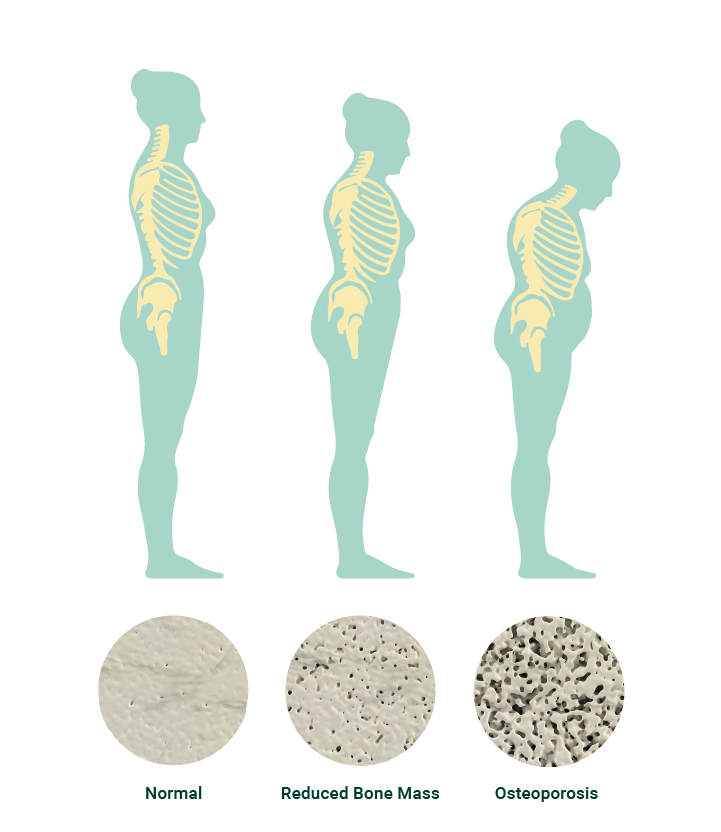
You might have come across the term “Dowager’s Hump,” also known as Kyphosis, which is pretty common among people with osteoporosis affecting their spine.
It’s that noticeable forward curve in the spine that can lead to a hunched posture and even cause fractures in the vertebrae, often referred to as “wedge fractures.” This happens when the front part of a spinal bone collapses, leading to that curved spine look.
What’s really surprising about these fractures is that they can be painless. That’s right, you could have a fracture in your spine and not even realize it.
So, how does this happen? Well, as your spine loses bone density, the bones become less solid and more porous, making them much easier to break. The simplest actions, like bending forward or leaning to one side, can cause these bones to fracture spontaneously.
Below is the visual effect of developing osteoporosis when it comes to vertebrae fractures. You will notice the loss of bone density with age and the slight curve of the spine.
If you’ve fractured a bone, or you have any of the visible signs of osteoporosis, it’s a good idea to arrange a DEXA scan to determine if the culprit is bone loss.
Bone Fracture Healing Process
There are many different types of fractures, but the good news is, they all follow the same bone fracture healing process.
Right after a fracture occurs, your bone kicks into repair mode and starts a natural healing journey. This journey can be broken down into five key stages, which we’ll go through next.6,7
Stage 1: Hematoma Formation
During the break, a hematoma is formed as blood vessels in and around the bone tissue are damaged as well. A hematoma is clotted blood that swells inside the bone tissue. The clot forms the temporary frame for subsequent healing.
Stage 2: Granulation Tissue Formation (Inflammation)
Within a few hours, inflammatory molecules enter the scene as your hematoma is reabsorbed. These molecules are your body’s first line of defense, with the job of cleaning out dead bone while preparing the fracture site for tissue, cartilage, and bone formation. This stage is the rebuilding of vessels and cells affected by the fracture.
Stage 3: Callus Formation
After about five days or so, a temporary soft callus is formed at the area of the bone fracture. The callus is made of newly formed fibroblasts (collagen-secreting cells), chondroblasts (cartilage-building cells), and osteoblasts (bone-building cells). This soft callus creates a foundation in which the bone can attempt to heal itself. In addition to the callus, a layer of woven bone begins to be laid down by stem cells. Capillaries and supporting blood vessels connect to the callus as the rebuilding process continues.
Stage 4: Consolidation
With the continued expression of cells that help to produce and break down cartilage and bone (chondroblasts, chondroclasts, osteoblasts, and osteoclasts), the soft callus is resorbed and begins to calcify. During the consolidation stage of healing, a stronger type of bone, called lamellar bone, replaces the woven bone. This stage typically starts within the first month of healing.
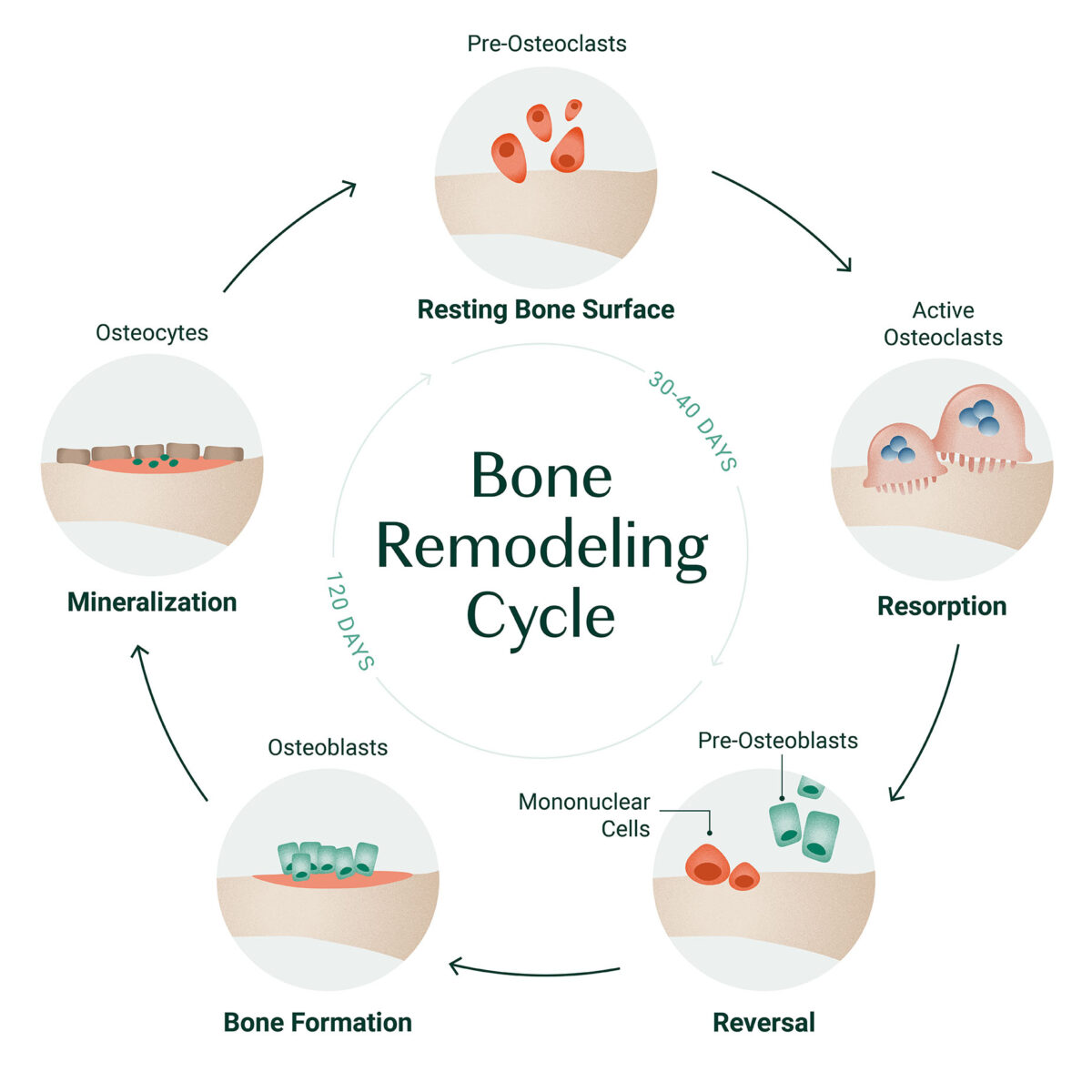
Stage 5: Bone Remodeling
By the end of the first month, the lamellar bone ultimately fills in the fracture site and aligns in the direction of the external forces on the bone. This stage is carried out primarily by osteoclasts (bone-resorbing cells) and osteoblasts (bone-building cells) and can last anywhere from a few months to a few years.
During the bone healing process, it’s advised that you be monitored by an approved healthcare provider. They will guide you and be able to tell you when you have reached the point during your recovery where you can start to incorporate weight-bearing exercises into your regimen. Weight-bearing exercises will continue to help the bone heal and remodel.
Symptoms of Bone Fractures
If you’re worried you might have a broken bone, keep an eye out for these common signs and symptoms:
- Pain
- Loss of Function
- Height loss
- Curved spine
- Swelling
- Bruising
- Bleeding
- Tenderness
- Limping
How To Diagnose a Bone Fracture
Wondering if you’ve got a broken bone? Sometimes, it’s super clear, like with a compound fracture where the bone is visible. But other times, it might not be so obvious.
Here’s what to do: Head straight to your doctor or the nearest emergency room. They’ve got the tools to figure out exactly what’s going on.
First off, your doctor will check you over with a physical exam and then probably suggest some imaging tests to see how bad the break is.
The go-to test is usually an X-ray. It’s great for confirming a fracture and showing where and how the bone has broken. If your doctor needs to check out the damage to the areas around the bone, like your ligaments and cartilage, an MRI might be in order. It gives a more detailed picture of those soft tissues.And in some cases, you might need a CT scan. This test gives an even more detailed view of your bones and the surrounding tissues, helping your doctor plan the best way to fix things up.
How To Treat Bone Fractures
After your doctor checks out your X-rays or other scans, they’ll lay out the best plan to get your bone healing properly. If it’s a simpler break, you might just need a splint or a cast to keep everything in place. But more serious fractures might require surgery.8
Whether you’re in a cast or recovering from surgery, there are steps you can take to accelerate your healing process:
Get Moving: A study examining 166 people who had surgery for broken tibia bones found something interesting. When these people started doing exercises that put weight on their leg early on, their bones healed faster. This was true even for those whose bones weren’t healing as expected.9

So, why does exercise help in this way? It’s all about improving blood flow and oxygen to the broken bone. Exercising makes your blood vessels wider, which lets more oxygen, nutrients, and special growth-promoting substances reach the area of the fracture. Moreover, exercise leads to the release of adenosine triphosphate (ATP), an important energy molecule. When bone cells in a lab are mechanically stimulated (in a way that mimics exercise), they release ATP, which encourages the formation of new bone. This step is crucial for the healing process.
There’s another important aspect of how exercise aids bone healing. Research has shown that osteocytes, a specific type of bone cell, get activated by the muscle contractions that occur during weight-bearing exercises. These osteocytes then send signals to other bone cells to create new, stronger bone tissue. This process is essential for mending the fracture, essentially helping to “patch” the broken parts of the bone together.10
Up Your Protein: Getting enough protein is key to healing a broken bone. But how much protein do we really need? The standard advice has been to consume 0.8 grams of protein per kilogram of body weight each day. But that’s the absolute minimum! This guideline was established over ten years ago mainly to avoid protein deficiency, not to optimize health.
Experts now believe that for the best health outcomes, especially for older adults and those healing from fractures, a higher protein intake is essential. Recent studies recommend consuming between 1 and 1.5 grams of protein per kilogram of body weight.12
Let’s break it down with an example: If an older adult weighs 140 pounds, they’d first convert their weight to kilograms by dividing by 2.2, giving them 64 kilograms. Multiplying this by 1.5 (for the maximum recommended intake) equals 96 grams of protein needed daily. To put it in perspective, a 3.5-ounce chicken breast contains about 30 grams of protein, so roughly three chicken breasts would meet this daily requirement.
Why is protein so crucial for bone repair? It’s all about the amino acids, which are the building blocks of our body. While our body can make some amino acids (the non-essential ones), there are nine essential amino acids that we must get from our diet because our body can’t produce them.
Animal-based foods like meat, fish, and dairy are “complete” proteins, meaning they contain all the essential amino acids. Plant-based proteins, found in grains, legumes, and vegetables, often lack one or more essential amino acids and are thus considered “incomplete.”
Remember, it’s important to include protein in every meal to support bone health and overall well-being. For more detailed information on protein sources and the link between protein and bone health, check out our Protein and Bone Health guide.
Get More Minerals: Most folks don’t get enough essential minerals from their diet. Beyond calcium, your bones need a specific combination of 13 minerals and vitamins. Getting enough of these bone-building nutrients is almost impossible with the typical Standard American Diet. Take copper as an example…
Copper is critical in synthesizing collagen, a key protein in bones and connective tissue. It’s one of the things that give your bones their strength and shape! So, if your body doesn’t get enough copper, it can’t make enough collagen, leading to weaker bones.
Besides helping with collagen, copper is also part of the bone mineralization process. This is where your bones get their hardness and strength from minerals. It plays a role in linking up collagen and elastin (another protein in your bones), ensuring your bones are both strong and flexible.13
The RDA for copper is 900 mcg, with oysters, kale, shiitake mushrooms, and dried prunes all providing rich sources of this nutrient. And while 900 mcg doesn’t sound like much as many as 1 in 4 Americans aren’t getting enough of this essential nutrient.14 And remember, copper is only 1 of the 13 minerals your bones need. You also need calcium, magnesium, potassium, phosphorus, boron, silica, manganese, vanadium, strontium, nickel, selenium, & zinc! And that’s not all! You also need vitamins D3, K2, and C. Lacking a single one of these essential nutrients can deplete your bone density and harm your fracture recovery. That’s why it’s important to supplement with a clinically supported, multi-nutrient bone building supplement, which also promotes bone healing.

Takeaway
Breaking a bone is something that can happen to anyone, no matter their age. But if you’re over 50 or have osteoporosis in your family, your risk of fractures goes up. If that sounds like you, it’s a good idea to chat with your doctor about checking your bone density. This can help you catch osteoporosis early, which means you can start taking steps to prevent fractures before they happen.
Want to stay in the loop with the latest tips on aging well and keeping your bones healthy? Sign up for the AlgaeCal Newsletter for all kinds of useful info.
FAQs
What causes broken bones?
A large number of bone fractures occur due to high force impact or stress: car accidents, falls from heights, playing on unsafe surfaces etc. However, some fractures may be caused by medical conditions that weaken the bones, such as osteoporosis or bone cancer.
How long does it take for a broken bone to heal?
In general, the most significant work in the bone healing process is completed in six to eight weeks, but speed can vary widely depending on the individual. One key factor is age. Adults, especially seniors, experience a much longer road to recovery than children. Nutritional status, medical conditions, and the location of the fracture also play a role.
What are the main types of bone fractures?
Two common types of bone fractures are simple and compound. Simple fractures describe a broken bone beneath the skin, while compound fractures occur when the broken bone pierces the skin.
What is the difference between broken bones and fractures?
Bone fractures and broken bones are two terms that describe the same thing. Fracture is a word that’s more commonly used in a medical setting, but these two can be used interchangeably.





Edwin Simpson
February 29, 2016 , 11:58 amI broke the nuckle of my little finger on Dec.13 last year. But I did not go to a Dr. until 6 weeks,later. They put a semi soft hard cast for 2 weeks than a brace for 4 weeks. But it achs and is slightly swollen and hand is numb little finger cannot straighten out. Or touch the next finger. I don’t think the fracture is healing right? What should I do?