Can Gluten Harm the Health of Your Bones?
Gluten, a protein found in wheat and a handful of other grains, is known to cause inflammation and digestive issues. What we’re learning, however, is that when your body reacts to gluten, it can negatively impact various systems in your body — bones included.
In this article, we’ll discuss how gluten can impact bone health and touch on a couple of other potentially dangerous compounds found in wheat. Then we’ll leave you with some simple tips for a healthy gluten-free lifestyle.
How Does Gluten Affect Bone Health?
To understand how gluten impacts bone health, we first have to start with your gut.
In 460 BC, Hippocrates, the father of western medicine, stated, “All disease begins in the gut.”
In 2010, Dr. Alessio Fasano put this major medical insight into modern-day terms, saying, “The gut is not like Las Vegas. What happens in the gut does not stay in the gut.”
Fasano was alluding to the fact that gluten disrupts gut function and, in the process, allows compounds that are supposed to stay within the gut barrier to leak into your blood. This process, called increased intestinal permeability, is not only an issue for those with celiac disease but occurs in approximately 80% of the population.
Today we’re learning that the impact of this disruption goes far beyond the gut and can cause chronic inflammation that promotes numerous degenerative diseases, including osteoporosis.
Zonulin & Intestinal Permeability
How exactly does gluten trigger intestinal permeability?
The culprit is a compound called zonulin. Zonulin is a protein in your gut that opens up the tight junctions between your intestinal cells.
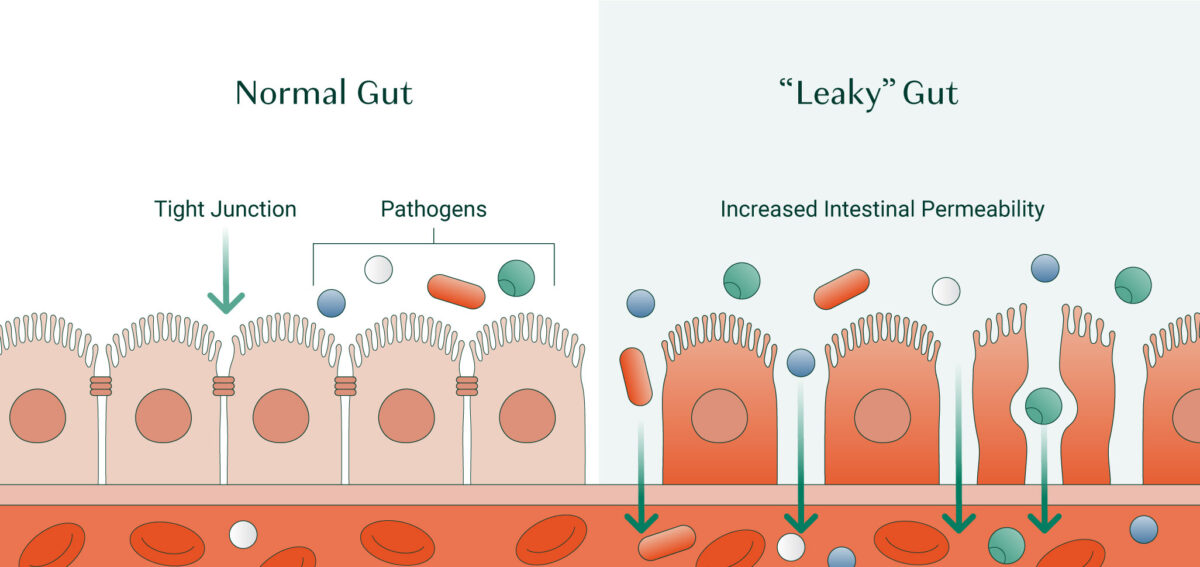
Zonulin’s job is to greatly increase intestinal permeability. In response to pathogenic organisms and toxins, zonulin opens up the walls of your intestines, encouraging fluids to pour into the intestinal tract. This triggers osmotic diarrhea to flush the offenders out of your body.
In response to wheat, the release of zonulin and increase in intestinal permeability is less dramatic – but it occurs every time during the day when you consume foods containing gluten. This means that throughout your day, gluten triggers the opening of your intestinal “doors” to allow whatever is in your gut – including unfriendly organisms like yeasts, unfriendly bacteria, molds, and incompletely digested proteins — to gain access to your bloodstream and invade your entire body.
Not surprisingly, this promotes chronic inflammation and the development of many diseases in which chronic inflammation plays a part –including osteoporosis, asthma, allergies, rheumatoid arthritis, fibromyalgia, cardiovascular, liver, and kidney disease[1][2].
Not everyone produces zonulin. About, 20% of the population doesn’t, and therefore is less affected by gluten. But be warned; even if you fall within that 20%, zonulin isn’t the only concern regarding gluten and bone health.
Other Bone-Destroying Mechanisms of Gluten
Gluten contains a polypeptide called α-gliadin, which is highly inflammatory and may instigate bone loss through several mechanisms, including:
- Cytotoxicity: instigating cell death[3].
- Immune activation: by modulating immunity, these polypeptides can inappropriately ramp up immune system responses[4][5].
- Proinflammatory messaging: α-gliadin instigates the release of a key proinflammatory messenger called IL-8 that jump-starts and then ramps up inflammatory immune responses[6].
In addition to the excessive inflammatory response that gluten can impose, many people with gluten sensitivity experience malabsorption due to impaired gut barrier function. For bones to grow strong and healthy, they require adequate levels of specific nutrients, including calcium and vitamin D. Even if you’re continuously consuming these nutrients, if your gut lining is damaged, you won’t be able to properly absorb and utilize them to maintain healthy bones.
Furthermore, studies show that when people with celiac disease consume gluten, it can create antibodies against a compound called Tissue Transglutaminase (tTG). Tissue transglutaminase is an enzyme that fixes damage in your body and plays a crucial role in bone renewal, The presence of antibodies for tTG is associated with decreased bone mineral density (BMD)[7].
The Difference Between Celiac Disease and Gluten Sensitivity
People often get confused about the difference between celiac disease and gluten sensitivity. While both of these conditions can present with similar symptoms, there are some distinct differences in the pathology and the treatment of celiac versus gluten sensitivity.
Celiac Disease
Celiac disease is a genetic, autoimmune disorder that causes your immune system to attack the lining of your small intestine when you consume gluten. Each time you consume gluten, the damage to your gut lining becomes worse, eventually impacting your ability to absorb and distribute nutrients into the bloodstream for your body to use[8].
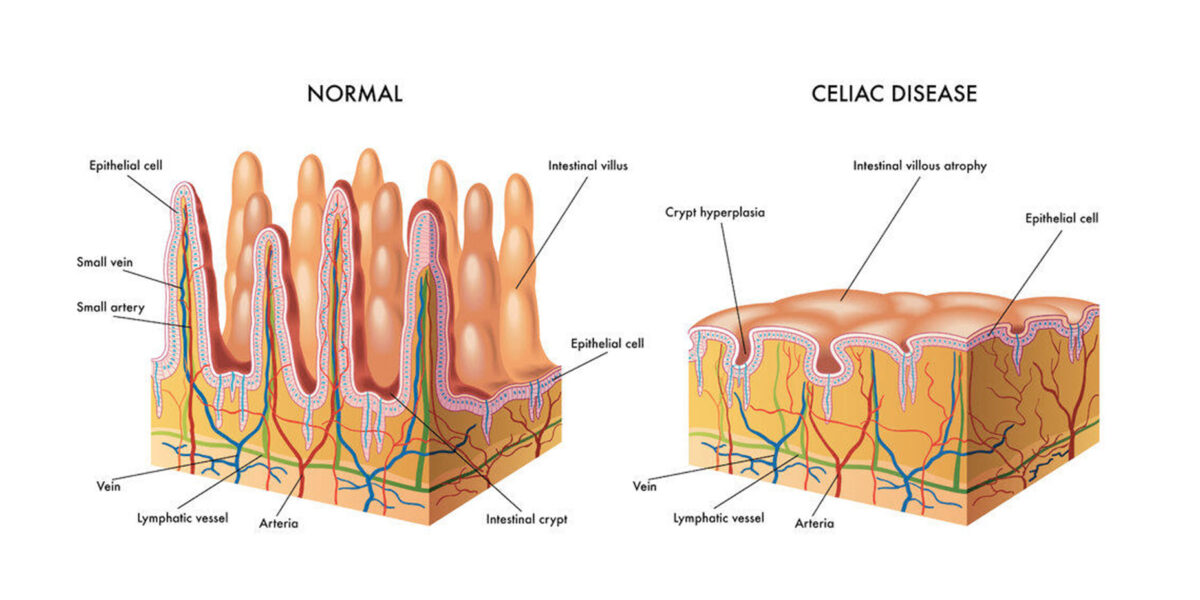
One of the issues with celiac disease is the overactivation of zonulin. For those with gluten sensitivity, the opening of your intestinal walls quickly reverses (within about four hours). However, for those with celiac disease, your intestinal wall can remain permeable and open until gluten has been strictly avoided and eliminated from your diet.
Over time, celiac disease can lead to serious malnutrition due to nutrient deficiencies and may lead to a range of symptoms including, but not limited to:
- Fatigue
- Constipation
- Abdominal bloating and pain
- Behavioral changes
- Arthritis
- Irritability
- Anemia
- Bone or joint pain
- Low bone density
The most common blood test for celiac disease is the Tissue Transglutaminase Antibodies (tTG-IgA) test. If you discover that you have celiac disease, the only treatment is to follow a gluten-free diet.
Non-Celiac Gluten Sensitivity
Non-Celiac Gluten Sensitivity (NCGS) is a condition in which people experience similar reactions to gluten as those with celiac disease, without the clinical markers.
Currently, 1% of the United States population has been diagnosed with celiac disease, but “Non-celiac gluten sensitivity” is thought to be present in far more people –up to 6% of the population. Furthermore, a Gallup poll conducted in July 2015 showed that 20% of Americans now opt for a gluten-free diet.
Researchers are still trying to pin down the exact mechanism behind gluten sensitivity, but several factors likely play a role, including the impact of gluten itself as well as modern food processing (which we’ll get into shortly).

Gluten sensitivity triggers a range of symptoms including[9][10]:
- Bloating
- Abdominal pain
- Epigastric pain
- Diarrhea
- Constipation
- Eczema and dermatitis/rashes
- Headache
- Brain fog and difficulty concentrating
- Fatigue
- Anxiety
- Depression
- Numbness in the legs, arms, or fingers
- Joint pain
One way to determine if you have gluten sensitivity is to ask your doctor about ordering a blood test to check for antigliadin antibodies IgG. Approximately 50% of patients who are gluten sensitive are positive for antigliadin antibodies of the IgA and/or IgG classes. However, if you’ve been following a gluten-free diet, you likely won’t show positive results because these antibodies tend to disappear quickly in the absence of gluten, along with gluten-sensitivity symptoms.
Therefore, the best way to determine if you have gluten sensitivity is to follow a strict gluten-free diet for a couple of months to see how you feel. It can be helpful to make notes and keep a journal to track your symptoms, and then after two months, try reintroducing gluten to see if you have a reaction.
The Rise of Gluten Sensitivity
In the last several decades, we’ve seen a sharp rise in gluten sensitivity as well as celiac disease. Why, all of a sudden, are we seeing such dramatic increases? Because wheat has been significantly “hybridized” and “deamidated” over the last 50 years.
Hybrid Wheat
Hybridization is a process of cross-breeding different varieties of wheat to strengthen the crop and increase its yield. The issue with hybrid wheat is that the process creates entirely new proteins that can alter gluten’s protein sequence by as much as 5%. These new proteins are hypothesized to be part of the reason that “modern” gluten is so highly inflammatory for so many people[11].
Deamidated Wheat
Another process that has changed the structure of gluten is deamination, which uses enzymes or acids to make gluten water-soluble. Deamidation is used extensively in the processed food industry to allow gluten to mix more easily with other food products. Unfortunately, this process also creates new-to-our-digestive-tract substances that, not surprisingly, generate a severe immune response in susceptible people[12].
Other Potentially Harmful Components of Wheat
Amylase-Trypsin Inhibitors
Amylase-trypsin inhibitors are a group of proteins found in wheat and other grain products that inhibit the activity of enzymes required for healthy digestion. The presence of ATIs is associated with an activated immune response and increased inflammation[13].
Fructans
Another potentially harmful compound in wheat is fructans, which are a type of carbohydrate known as oligosaccharides. Oligosaccharides can be fermented in the small intestine, leading to various digestive issues. You may have heard of the FODMAP Diet. FODMAP is an acronym for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols[14].
Many individuals with inflammatory bowel disease are told to see if following a low FODMAP diet will help manage their symptoms as this diet avoids foods rich in fermentable compounds that can create digestive disturbances in susceptible people[15].
Along with wheat, other foods that are high in fructans include:
- Grains (spelt, rye, barley)
- Fruit (watermelon, grapes, nectarines, grapefruit, bananas)
- Vegetables (brussels sprouts, cabbage, asparagus, beets, fennel, artichoke)
- Beans (kidney, mung, soy, lima, navy)
- Nuts (cashews and pistachios)
- Garlic
- Chicory root
Tips For Living Gluten-Free
Living gluten-free is much easier today than it was even just ten years ago. That said, you still need to be aware of hidden sources of gluten, as well as which grains other than wheat contain gluten.
Avoid Hidden Sources of Gluten
Some of the most common hidden sources of gluten include:
- Oats that have been harvested with wheat (gluten-free oats are widely available)
- Sauces (marinades, soy sauce, salad dressing, look for gluten-free versions)
- Drug fillers
- Processed meats
- Shared food preparation (e.g., toaster, deep fryer, pasta pot)
It’s also important to remember that your skin is highly porous, and you can absorb allergens when used topically. Some lipsticks, body lotions, shampoos, etc., contain gluten, so be wary of your choices. The good news is that many companies are now including “gluten-free” on their label to indicate that their products are safe for gluten-sensitive consumers.

Which Grains Are Gluten-Free?
While you’ll have to avoid gluten-containing grains like wheat, barley, rye, and spelt, there are plenty of delicious gluten-free alternatives, including:
- Corn
- Rice
- Potato
- Amaranth
- Buckwheat
- Millet
- Sorghum
- Teff
- Quinoa
(If you like to make your own bread, give this Gluten-Free Sourdough Starter a try!)
Consider Other Food Sensitivities
Many people find that if they are sensitive to one food, they may also be sensitive to other common allergens. If you’ve tried eliminating gluten and still notice symptoms, it could be helpful to follow a more substantial elimination diet that includes other common triggers such as eggs, dairy, soy, and corn.
You can also have blood work drawn to determine food sensitivities, but blood work is notoriously less reliable than an elimination diet.
Takeaway
Whether your body reacts to wheat-containing foods or not, gluten and the other potentially dangerous compounds in wheat are best avoided if you want to protect the integrity of your bones.
Even those that are able to tolerate gluten just fine will likely find that removing wheat can enhance their overall health and well-being. This may not have been the case 100 years ago, but with our modern food processing practices, the wheat we consume today is less compatible with the human system.
The good news is that avoiding gluten is easier today than ever before. With a widespread understanding of the dangers of wheat, we’re seeing more and more gluten alternatives that can replace your standard wheat-containing items.
FAQs
Does gluten affect your bones?
Yes, gluten can cause inflammation through several pathways that may ultimately impact bone health and remodeling. This is especially the case in celiac disease, but those who are only “gluten sensitive” are also at risk for inflammatory-related bone issues.
Does a gluten-free diet help osteoporosis?
Due to the inflammatory impact of gluten, removing this protein from your diet may improve osteoporosis by reducing inflammation and enhancing bone-supportive nutrient absorption.
What is the mechanism of osteoporosis in celiac disease?
Osteoporosis is one of the many complications of celiac disease due, in part, to antibodies that are generated against a compound called Tissue Transglutaminase (tTG). This compound plays a crucial role in bone remodeling, and the presence of its antibodies is associated with decreased bone mineral density (BMD).
Can non-celiac gluten sensitivity cause osteoporosis?
People with non-celiac gluten sensitivity (NCGS) are at risk for osteoporosis due to impaired intestinal barrier function interfering with the absorption of key nutrients for bone health, such as calcium and vitamin D. Furthermore, NCGS can produce widespread inflammation that can increase osteoclast activation and the rate of bone loss. .
References
- Fasano, Alessio. “Zonulin, regulation of tight junctions, and autoimmune diseases.” Annals of the New York Academy of Sciences 1258.1 (2012): 25-33.
- Fasano, Alessio. “All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases.” F1000Research 9 (2020).
- Sakly, W., et al. “A role for tissue transglutaminase in α-gliadin peptide cytotoxicity.” Clinical & Experimental Immunology 146.3 (2006): 550-558.
- Barone, Maria Vittoria, Riccardo Troncone, and Salvatore Auricchio. “Gliadin peptides as triggers of the proliferative and stress/innate immune response of the celiac small intestinal mucosa.” International journal of molecular sciences 15.11 (2014): 20518-20537.
- Nanayakkara, Merlin, et al. “An undigested gliadin peptide activates innate immunity and proliferative signaling in enterocytes: the role in celiac disease.” The American journal of clinical nutrition 98.4 (2013): 1123-1135.
- Jelı́nková, Lenka, et al. “Gliadin stimulates human monocytes to production of IL-8 and TNF-α through a mechanism involving NF-κB.” FEBS letters 571.1-3 (2004): 81-85.
- Agardh, Daniel, et al. “Coeliac disease-specific tissue transglutaminase autoantibodies are associated with osteoporosis and related fractures in middle-aged women.” Scandinavian journal of gastroenterology 44.5 (2009): 571-578.
- https://celiac.org/
- Catassi, Carlo, et al. “Non-celiac gluten sensitivity: the new frontier of gluten related disorders.” Nutrients 5.10 (2013): 3839-3853.
- https://celiac.org/about-celiac-disease/related-conditions/non-celiac-wheat-gluten-sensitivity/
- de Lorgeril, Michel, and Patricia Salen. “Gluten and wheat intolerance today: are modern wheat strains involved?.” International journal of food sciences and nutrition 65.5 (2014): 577-581.
- Denery‐Papini, Sandra, et al. “Allergy to deamidated gluten in patients tolerant to wheat: specific epitopes linked to deamidation.” Allergy 67.8 (2012): 1023-1032.
- Geisslitz, Sabrina, et al. “Wheat amylase/trypsin inhibitors (ATIs): occurrence, function and health aspects.” European Journal of Nutrition 61.6 (2022): 2873-2880.
- Gibson, Peter R., and Susan J. Shepherd. “Evidence‐based dietary management of functional gastrointestinal symptoms: the FODMAP approach.” Journal of gastroenterology and hepatology 25.2 (2010): 252-258.
- Altobelli, Emma, et al. “Low-FODMAP diet improves irritable bowel syndrome symptoms: a meta-analysis.” Nutrients 9.9 (2017): 940.






Francoise
August 17, 2016 , 4:02 amRecently a friend of mine who has ordered Algaecal + Strontium for the first time, told me her french GP recommended she does not take Strontium due to her hypertension and related risks such as cardiovascular diseases. Her doctor commented that Strontium (of the french version) has been taken off the shelves for this reason. I tried to persuade her that your Strontium is different, to no avail. Would you please comment on the safety of Strontium for people with hypertension. Thank you very much.
ps: I have myself taken your products (both) for 7 years and my increased bone density has left my GYN doctor amazed, but I do not have high blood pressure.
Francoise.