Most people are aware of osteoporosis; however, its sister bone disease, osteomalacia, gets much less press.
There are some distinct differences between these two conditions, although both lead to the same result – weak bones that are prone to break.
In this article, we’ll explore what osteomalacia is, why it happens, and the differences between osteomalacia and osteoporosis.
What Is Osteomalacia?
Osteomalacia (which means “soft bones”) is a condition that impairs your bone’s ability to mineralize, and therefore harden properly.
To understand the pathology of osteomalacia, we first need to look at two primary components of your bone:
- The bone matrix (made up primarily of collagen)
- Minerals (deposited in the bone matrix, creating strength and integrity)
Your bones are constantly going through a process known as bone remodeling, where old bone is broken down, and new bone grows in its place. Osteoclasts are a type of bone cell that helps to break down bone, while osteoblasts work to remineralize the bone matrix. This process keeps your bones healthy and strong, and when interfered with, it can create issues such as osteoporosis and osteomalacia.
In the case of osteomalacia, a lack of vitamin D results in demineralization of the bone matrix.
Here’s why: Vitamin D is essential for calcium absorption in the body, so low vitamin D means reduced intestinal absorption of calcium. Our bodies must tightly regulate blood calcium to support vital functions (such as generating a heartbeat), so when your blood calcium levels drop too low (in this case, from low intestinal absorption), your body looks for backup in your bones[1].
As a result, the composition of your bone shifts and becomes more collagenous and less mineralized, making them weak and quite literally “softer.” This interferes with bone remodeling, as bones with osteomalacia tend to break down faster than they can rebuild.
In children, vitamin D deficiency causes a similar issue called “rickets,” where tissue near the ends of long bones becomes weakened, which can lead to bone deformities. Luckily, we rarely see rickets anymore since the fortification of milk back in the 1930s[2].

Healthy bones start here
AlgaeCal provides the industry’s leading supplements and support designed to meet you at every stage of your bone-health journey. Find the right choice for you.
Osteomalacia vs. Osteoporosis
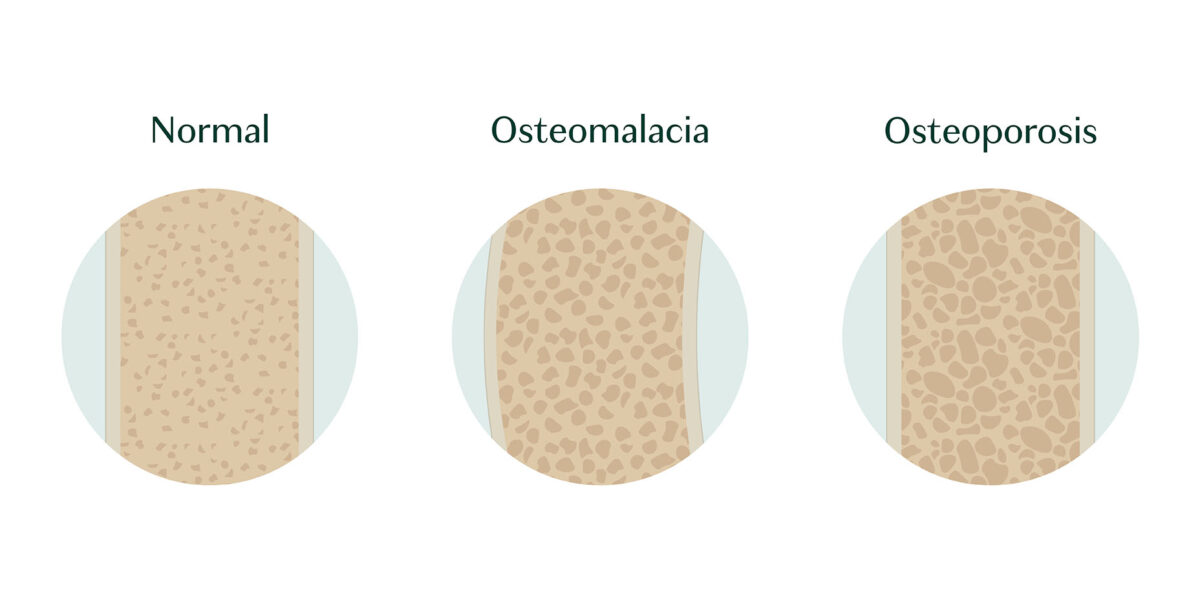
The primary difference between osteomalacia and osteoporosis comes down to how they impact bone structure.
In osteomalacia, lack of mineralization causes the composition of bone to shift more heavily toward collagen instead of a balance between collagen and minerals. Collagen is much softer than minerals, which ultimately means that your bones become soft and more prone to break.
In osteoporosis, your bone mineral density decreases over time, making the honeycomb-like structure of your bones more fragile. This can create weak, brittle bones that are also more prone to fracture.
Now let’s dive in a bit deeper to parse out these two conditions.
Osteomalacia Causes
The most common cause of osteomalacia is a vitamin D deficiency. Vitamin D is essential for calcium absorption, so when this nutrient is deficient, calcium deficiency often follows.
Vitamin D deficiency can result from several factors, including:
- Diet: While there are some food sources of vitamin D such as eggs, fish, and fortified milk and juices, it’s still a challenge to get enough.
- Lack of sunlight: A much more efficient way for your body to synthesize vitamin D is actually through sunlight; the problem is that in our modern society, we typically don’t get enough of it. While our ancestors would have been outside all day, with moments in the shade here and there, today most people work indoors and avoid too much sun exposure due to inclement weather. Many people also avoid the sun due to the risk of melanoma[3].
- Liver or kidney disease: Both of these conditions may inhibit the proper absorption of vitamin D[4].
- Absorption problems: Gastrointestinal disorders like Crohn’s disease, celiac disease, and IBD can make it more challenging to absorb vitamin D through the diet.
- Certain medications: Some pharmaceutical medications may inhibit the absorption or production of vitamin D.
Osteomalacia may also be caused by mineral deficiencies, specifically calcium and phosphorus, but this is much less common.

Osteoporosis Causes
The most common cause of osteoporosis is the combination of aging along with hormonal changes. As a young person, up until the age of about 30, you create more bone than you lose in the bone remodeling process.
However, once you get into your late 30s, bone breakdown begins to outpace the regrowth process[5]. This is typically not an issue for people in their 30s or 40s, but once you hit your 50s, another factor comes into play – hormones.
Women are particularly susceptible to osteoporosis due to the sharp decline in estrogen that happens with menopause. Estrogen is a vital hormone for regulating calcium and directly influences the bone remodeling process. Therefore, when estrogen levels start to plummet, bone health can take a hit[6][7][8].
Declining testosterone in men also impacts bone health. This is typically more gradual than estrogen in women but can be affected by medications and lifestyle factors[9]
Furthermore, some existing conditions that impair proper nutrient utilization may also interfere with the bone remodeling process, such as digestive dysfunction (IBD, celiac, Crohn’s), issues with the thyroid or parathyroid gland, and certain medications[10][11][12].
And of course, nutrition always plays a crucial role in bone health. Your diet is the primary source of the building blocks that your body needs in order to make bone. If you aren’t getting enough nutrients such as calcium and vitamin D through your diet or supplement regimen it will increase your risk of osteoporosis[13][14].

Osteomalacia Symptoms
Osteomalacia can present with a range of symptoms that indicate that your bone health is deteriorating. Common symptoms include[15]:
- Muscle weakness
- Difficulty walking
- Pain in the bones, especially around the hips, back, and legs
- Fractured bones due to minimal trauma
Osteoporosis Symptoms
Osteoporosis is called the silent disease because it may not present with symptoms at first as this condition typically evolves slowly over time. In fact, most people don’t even realize they have osteoporosis until they experience their first fracture. With that being said, there are some signs to watch out for, including[16]:
- Postural changes (hunched posture, bending forward)
- Losing height (getting shorter by an inch or more)
- Shortness of breath and pain with coughing (due to smaller lung capacity)
- Pain in the lower back
Osteomalacia Treatments
Since the root cause of osteomalacia is usually low vitamin D, the most effective treatment is getting your vitamin D levels back up. This can be accomplished through more direct sunlight, consuming more vitamin-D-rich foods, or, most commonly, taking a vitamin D supplement.
If the osteomalacia results from a mineral deficiency such as calcium or phosphorus, then you would likely be advised to supplement with minerals.
In most cases, supplementing with both minerals and vitamin D is a good measure to take to provide your body with everything it needs to turn things around.

Osteoporosis Treatments
The osteoporosis treatment plan depends largely on your bone mineral density scan results. However, no matter what stage you’re in, you’ll likely be directed towards supplements that include vitamin D, calcium, and other bone-building nutrients.
Furthermore, physical activity, especially weight-bearing exercise, helps to promote bone strength. Amazingly, muscles communicate with bones through over 600 different molecular connections. This is known as “muscle-bone crosstalk.” Yoga, in particular, is a fantastic option for people with osteoporosis because while it’s gentle on the joints, it also generates forces up to 10 times greater than gravity.
Many people that are diagnosed with osteoporosis find the combination of supplements plus more physical activity do the trick in turning bone health around.
In some cases, your doctor might recommend medications specific to your condition. With that being said, supplements that include bone-building nutrients are helpful at any stage of osteoporosis.
Summary: Osteomalacia Vs. Osteoporosis
| Osteomalacia | Osteoporosis | |
| Causes | The most common cause of osteomalacia is vitamin D deficiency, however other mineral deficiencies may also contribute. | Aging is the most common risk factor for osteoporosis, coupled with hormonal changes and nutrient deficiencies which impact bone health. |
| Symptoms | The most common symptoms of osteomalacia include: – Muscle weakness – Difficulty walking – Pain in the bones, especially around the hips, back, and legs – Fractured bones due to minimal trauma | Osteoporosis is known as the “silent disease” because most people don’t even know they have it until they have their first fracture. Some signs to watch for are postural changes, losing height, lower back pain, and shortness of breath. |
| Treatments | Since vitamin D deficiency is most frequently the driving factor behind osteomalacia, increasing vitamin D is often enough to turn things around. This can be accomplished by taking vitamin D supplements, increasing vitamin D in the diet, and getting more natural sunlight. You may also want to increase your intake of calcium and phosphorus as these two minerals play a crucial role in bone health. | The treatment plan for osteoporosis depends on the results of your bone density scan. Both physical activity and nutrients that support bone health (like vitamin D, calcium, and magnesium) can help to rebuild and strengthen bone. In the later stages of the disease you may be directed towards certain medications. |
Takeaway
Although osteoporosis and osteomalacia present differently, they both can stem from nutrient deficiencies and result in bone fractures.
As we get on in the years, it becomes increasingly crucial that we maintain our lifestyle habits such as staying active and getting bone-building nutrients into our diet.
Bone disease can sneak up on you, so be sure that you’re talking with your doctor about bone health exams.
Sign up for the AlgaeCal Newsletter for more tips and tricks to help you age gracefully and healthily.
FAQs
What is the difference between osteomalacia and osteoporosis?
The primary difference between osteomalacia and osteoporosis is how they impact bone structure. In osteomalacia, lack of mineralization causes the composition of bone to shift more heavily toward collagen instead of a balance between collagen and minerals. In osteoporosis, your bone mineral density decreases over time, making the honeycomb-like structure of your bones more fragile.
How are osteomalacia and osteoporosis similar?
Both osteomalacia and osteoporosis involve structural changes to your bones, making them weak and more prone to fracture.
What is the main cause of osteomalacia?
Lack of vitamin D is the primary cause of osteomalacia. When vitamin D is low, your body doesn’t absorb calcium well, which means that your bones become depleted of calcium. As a result, the composition of your bone shifts and becomes more collagenous and less mineralized.
What are the symptoms of osteomalacia?
Common symptoms of osteomalacia include muscle weakness, difficulty walking, pain in the bones (particularly around the hips, back, and legs), and easily fractured bones.
References
- https://www.ncbi.nlm.nih.gov/books/NBK551616/
- Walker, Alfredo, Dina El Demellawy, and Jorge Davila. “Rickets: historical, epidemiological, pathophysiological, and pathological perspectives.” Academic forensic pathology 7.2 (2017): 240-262.
- Wacker, Matthias, and Michael F. Holick. “Sunlight and Vitamin D: A global perspective for health.” Dermato-endocrinology 5.1 (2013): 51-108.
- Arteh, Jihad, Srilakshmi Narra, and Satheesh Nair. “Prevalence of vitamin D deficiency in chronic liver disease.” Digestive diseases and sciences 55.9 (2010): 2624-2628.
- https://my.clevelandclinic.org/health/diseases/4443-osteoporosis
- Ji, Meng-Xia, and Qi Yu. “Primary osteoporosis in postmenopausal women.” Chronic diseases and translational medicine 1.01 (2015): 9-13.
- McIlroy, Janet, et al. “Lesson of the week Oestrogen and calcium homeostasis in women with hypoparathyroidism.” BMJ 319.7219 (1999): 1252-1253.
- Khosla, Sundeep, Merry Jo Oursler, and David G. Monroe. “Estrogen and the skeleton.” Trends in Endocrinology & Metabolism 23.11 (2012): 576-581.
- https://www.spine-health.com/conditions/osteoporosis/testosterone-deficiency-and-osteoporosis
- https://www.endocrineweb.com/conditions/parathyroid/osteoporosis-parathyroid-disease
- Katz, Seymour, and Stuart Weinerman. “Osteoporosis and gastrointestinal disease.” Gastroenterology & hepatology 6.8 (2010): 506.
- Delitala, Alessandro P., Angelo Scuteri, and Carlo Doria. “Thyroid hormone diseases and osteoporosis.” Journal of clinical medicine 9.4 (2020): 1034.
- Kim, Kyoung Min, et al. “Interactions between dietary calcium intake and bone mineral density or bone geometry in a low calcium intake population (KNHANES IV 2008–2010).” The Journal of Clinical Endocrinology & Metabolism 99.7 (2014): 2409-2417.
- Sunyecz, John A. “The use of calcium and vitamin D in the management of osteoporosis.” Therapeutics and clinical risk management 4.4 (2008): 827.
- https://my.clevelandclinic.org/health/diseases/13017-osteomalacia
- https://my.clevelandclinic.org/health/diseases/4443-osteoporosis






Merilyn Green
April 18, 2023 , 11:33 pmThank you very much for this article. it agrees with things that I have read elsewhere, but puts it together so it’s clearer to understand. It was very helpful.