If you believe what you’ve read about menopause, you may assume that you’ll have to say goodbye to well-rested sleeps, your normal calorie-burning metabolism, and your sex drive. Not true!
This midlife transition doesn’t have to be the end of anything.
While menopause typically has negative connotations, this article will hopefully provide insights into new options that can help set you free to enjoy this time in your life. How so?
By giving you the science-backed research on what to expect. And equipping you with the knowledge to naturally solve menopause’s challenges.
Challenges like hot flashes (I prefer to think of them as power surges!), night sweats, a drop in libido, increased susceptibility to inflammation, and dry skin. Plus mood changes (not surprising if hot flashes wake you up sweating several times a night), and an increase in bone loss are possible, not guaranteed, occurrences during this time.
The really good news here is that all these menopause-associated symptoms are naturally treatable and preventable. It really is possible to sail through menopause with none of them and to emerge with no lasting changes except liberation from having to endure a monthly period.
With the information you need to optimize your health through this period of transition and beyond it, there’s no limit to what your body can do… and when it comes to menopause, your mindset can make a big difference.
In fact, research shows that what you believe about menopause can actually affect your experience. Women with more negative attitudes towards menopause generally report more symptoms during their menopausal transition.

What is Menopause?
Menopause is a natural part of the aging process during which a woman transitions from her years of potential childbearing to her fully mature years free of this responsibility.
It’s important to recognize that a woman’s reproductive years are only one stage of her life. Before menarche, a young girl’s first period, she is unable to bear children. After menopause as well, the potential for childbearing ceases. One of the first observational changes that signals this change during menopause is the gradual tapering off and final ceasing of menstrual periods.
Despite this process being natural, several menopausal symptoms may occur. Hot flashes and night sweats are the most common symptoms. Along with increased susceptibility to dry skin, including vaginal dryness, chronic inflammation, cardiovascular disease and loss of bone mineral density.
Although menopause is a normal life transition, individual experiences vary greatly. Some sail through menopause with nary a symptom. Others experience only a few for a short time, and some may need medical advice to manage their symptoms.
Fortunately, if you find yourself in this last category, today, no woman needs to experience any of these unpleasant symptoms.
The 4 Stages of Menopause
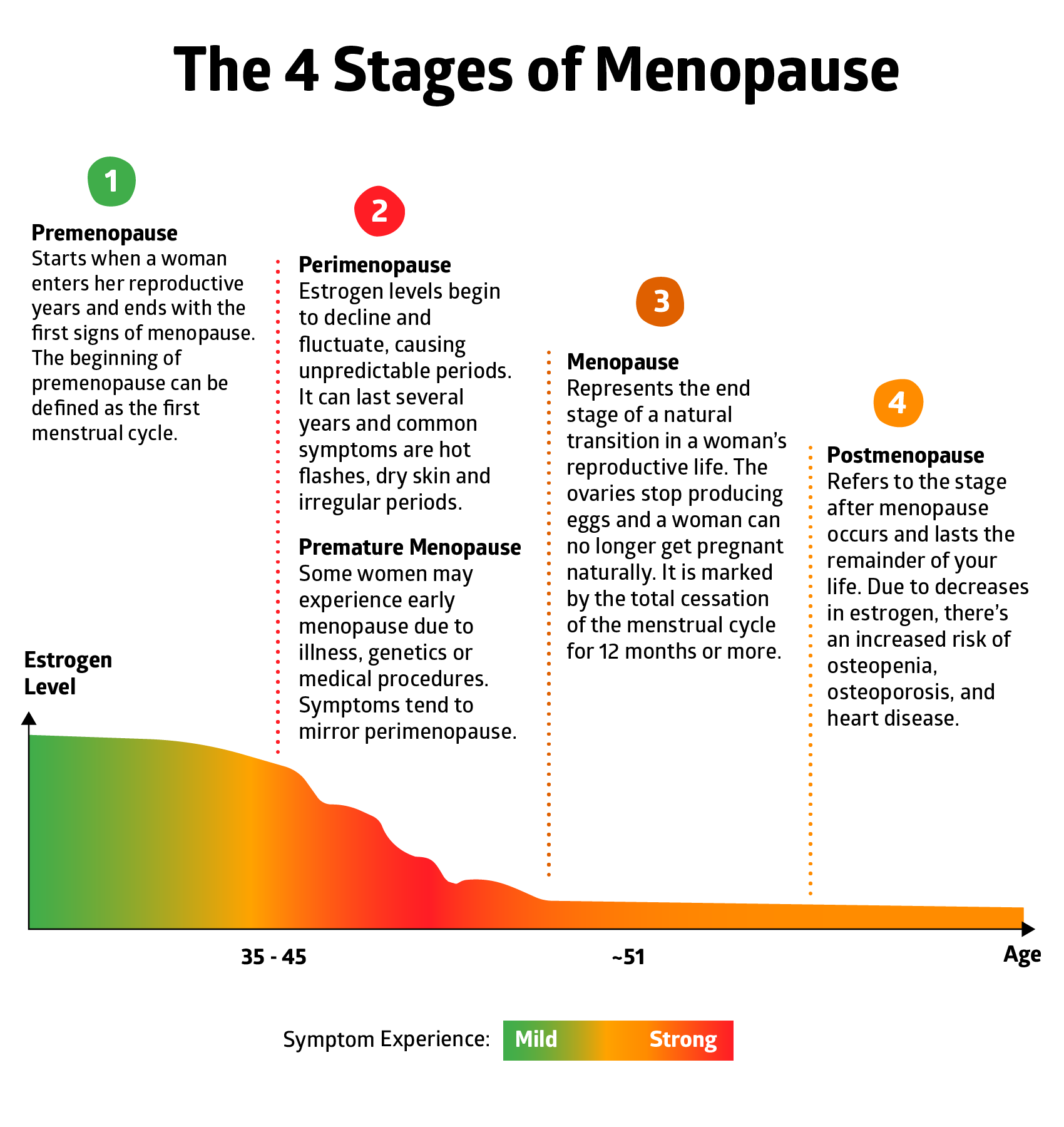
There are four stages of the menopausal transition: premenopause, perimenopause, menopause, and postmenopause. In addition, some women may also experience early or “premature” menopause, which occurs before the natural aging process.
Let’s look at each of the four stages…
Premenopause
Premenopause starts when an adolescent girl enters her reproductive years and ends with the first signs of menopause, which usually begin to appear between the ages of 48-52.
Perimenopause
Literally means “around menopause.” It’s also referred to as the “menopausal transition.”
This is the time when a woman’s body begins to shift from regular ovulation cycles and a monthly menstrual period to menopausal symptoms that may include: hot flashes, night sweats, infertility, vaginal dryness, and absence of menstruation. Women typically begin to experience this stage in their mid-40s.
Early or “Premature” Menopause
In the U.S., the average age for “natural” menopause is 52 years old. However, due to illness, smoking, medical procedures or genetics, some women may go through menopause early. Early menopause refers to onset before age 40. There are several known causes of early menopause, including:
- Genetics: If your mother or grandmother went through menopause early, you may have an increased chance of the same.
- Chromosome Defects: Two functioning chromosomes appear to be necessary for normal ovarian function. In a rare genetic condition called Turner Syndrome, the loss of the complete or near-complete second X chromosome occurs. This causes the ovaries to not function properly and typically leads to early menopause.
- Smoking: Smoking has anti-estrogen effects and promotes early menopause.
- Being too thin: Estrogen is stored in your fat tissues, so if you’re overly thin, you have fewer estrogen stores. Women who have a very low Body Mass Index (BMI) may be at risk of early menopause.
- Excessive exercise or lack of exercise: Some research suggests that either may promote early menopause.
- Excessive sun exposure or a lack of sun exposure: Again, some research suggests either may contribute to early menopause.
- Autoimmune diseases: Inflammation caused by autoimmune diseases can affect the ovaries. Early menopause can be a symptom of rheumatoid arthritis or thyroid disease.
- Epilepsy: Women with this seizure disorder that stems from the brain are more likely to experience early menopause. One study published in the journal Epilepsia found that women with epilepsy had an increased risk of developing premature ovarian failure.
- Procedures: A hysterectomy (removal of all or portion of the uterus) and/or an oophorectomy (removal of ovaries) will lead to early menopause.
- Treatments: Chemotherapy, hormone therapies, radiation and cancer treatments can contribute to early menopause.
While premature menopause is usually the result of one or more of the causes above, it can also occur naturally in some cases. Premature menopause symptoms are typically the same as natural menopause symptoms.
Menopause
This is the conclusion of the natural transition in a woman’s reproductive life. It’s the point where progesterone and estrogen production decrease permanently to low levels. The ovaries stop producing eggs, and a woman is no longer able to become pregnant, naturally. Menopause is officially marked by the total cessation of the menstrual cycle for 12 months or more. In other words, not having a period for at least 12 months in a row.
On average, menopause occurs around age 52 in the United States but varies from woman to woman.
Menopause-associated symptoms may never occur or can last for several months or even years, depending on the individual. With the exception of irregular periods, all the following common signs and symptoms can be prevented or effectively treated, naturally:
- Irregular Periods
- Vaginal Dryness
- Loss of Libido
- Hot Flashes
- Insomnia
- Urinary Incontinence
- Mood Changes
- Memory and Cognitive Function
- Hair Loss
- Decreased Breast Fullness
- Skin Issues
- Weight Gain
- Bone Loss
For a more in-depth and expanded version of menopause symptoms, check out: 13 Common Signs and Symptoms of Menopause.
Postmenopause
These are the years after menopause. From here on, a woman is postmenopausal for the rest of her life. A woman is considered postmenopausal when she has not had a menstrual period for a full year (12 months).
If you’re concerned about the possibility of an unwanted pregnancy, you can confirm you’re postmenopausal with a blood test called the follicle stimulating hormone (FSH) test. When a woman’s FSH level is consistently elevated to 30 mIU/mL or higher, and she has not had a menstrual period for a year, it’s generally accepted that she has reached menopause. However, using this test is not routine or needed for the vast majority of women.
The symptoms that began in perimenopause may continue past menopause, and without taking steps to support youthful function, many of them will remain.
Due to the significant decrease in estrogen and progesterone production, and the resulting increase in susceptibility to chronic inflammation, after menopause, women must take extra self-care steps to reduce our increased risk for heart disease and bone loss.
That’s why an anti-inflammatory lifestyle that includes regular, weight-bearing physical activity and an anti-inflammatory diet, along with key supplements that lower inflammation and ensure nutrient needs are fully met, become more important than ever.

Diagnosis of Menopause
In most cases, menopause is self-diagnosed with evident changes like hot flashes and 12 months without a menstrual period.
As you experience changes and symptoms, it’s best to get confirmation. Schedule a full physical with your healthcare provider to make sure that you are experiencing menopause. It’s a good idea to err on the safe side and do this because the signs and symptoms of menopause may mimic those of other health conditions, like hypothyroidism. Bloodwork and an exam can help rule out other conditions.
There are primarily 2 different types of testing: vaginal pH swab and FSH (follicle-stimulating hormone) levels.
- Vaginal pH Test: During reproductive years, a vaginal pH is around 4.5. During menopause, it rises to around 6.
- Follicle-Stimulating Hormone (FSH): During menopause, FSH rises and estrogen levels fall. Healthcare providers may check both to assess menopause. These levels may be measured more than once over the course of perimenopause for accuracy.
When diagnosing menopause, health care providers will assess age and menstrual patterns in addition to vaginal pH and bloodwork.
Because the signs and symptoms of menopause can mirror those of hypothyroidism, your healthcare provider may check your thyroid hormones as well.
Due to a decrease in estrogen levels during menopause, there’s also an increase in risk for heart disease and a decline in bone mineral density. It’s common for your healthcare provider to check your blood lipid profile, as well as recommend a bone density scan.
Menopause Complications
Menopause can result in an increased risk of certain health conditions including:
- Cardiovascular Disease: Cardiovascular disease (CVD) risk increases because decreased estrogen levels result in an increase in systemic inflammation and may adversely affect overall metabolism and cardiovascular function.
- Sexual Function: Vaginal dryness can occur during menopause due to decreased estrogen production. Since dryness can lead to vaginal pain during sex, the use of lubricants or topically applied estrogen creams is often recommended.
- Weight Gain: Metabolism may slow for women during menopause, which can lead to weight gain. Other factors like stress and lack of sleep during this time may also contribute to weight maintenance issues.
- Urinary Incontinence: You may experience frequent and abrupt urges to urinate, resulting in an involuntary loss of urine. Coughing, lifting or laughing can also cause urinary incontinence. You can strengthen your pelvic floor muscles with Kegel exercises.
- Osteoporosis: On average, women may lose up to 10% of their total bone mass during their menopausal transition! Then, added risk factors of osteoporosis like family history, lifestyle and poor diet can lead to excess bone loss of up to 20%.
As your production of estrogen and progesterone declines during menopause, your bone density will take a toll. The next section will show you exactly how menopause affects your bones.
3 Ways Menopause Affects Your Bones
The following trio can make for dangerous bone health conditions:
Hormonal Fluctuations
Hormones regulate the activity of cells and tissues in your organs. It’s essential that your body produces balanced hormones for overall health and well-being. However, during menopause, your fracture risk increases due to extreme hormonal changes. Why? These hormone changes disrupt your body’s natural bone-building process.
Estrogen, progesterone, and testosterone are hormones produced by the ovaries. The production of these three hormones changes and fluctuates during your mid-life years and can increase your risk of bone loss.
Hormones During Menopause
| Estrogen | Progesterone | Testosterone | |
|---|---|---|---|
| What is it? | Promotes the growth of tissues and ensures their function. It also decreases the perception of pain, increases HDL (good cholesterol) and preserves bone mass. | Is made primarily by your ovaries and plays a role in pregnancy.It ensures the function and development of the reproductive tract and breasts, but one of its most important roles is to balance the effects of estrogen.
It’s also a diuretic (promotes the increased production of urine), and it builds bone and benefits your cardiovascular system. |
A male androgen hormone produced at lower levels in women.It also builds bone and muscle, strengthens ligaments, assists brain function and boosts libido in both men and women.
Testosterone levels can influence sleep quality and stamina. It also has protective effects against cardiovascular diseases in women and men. |
| How does menopause affect this hormone? | Levels can fluctuate during menopause, leading to a decrease in estrogen production. This results in an increased risk of low bone density, osteopenia, and osteoporosis.Due to estrogen depletion, women are also at an increased risk of cardiovascular issues like strokes and heart attacks. | Menopause may cause low levels of progesterone, which results in abnormal menstrual cycles (periods may become irregular, longer and heavier). | Testosterone levels decline with age and gradually fall before menopause.Testosterone levels in women in their 40s tend to be half of those in their 20s. |
- Estrogen plays an important role in the regulation of bone turnover. During menopause, the ovaries decrease the production of estrogen. Estrogen deficiency can induce cortical (hard outer shell of the bone) and trabecular (spongy inside) bone loss. This increase in bone resorption can lead to the destruction of bone architecture, bone loss, and microfractures. Estrogen and calcium also have a relationship when it comes to bone health. Estrogen supports intestinal absorption of calcium. So having low estrogen levels can negatively impact the amount of calcium you’re able to absorb.
- Progesterone, like estrogen, plays an important role in bone turnover and bone formation. Because osteoporosis is primarily considered a result of estrogen deficiency, less emphasis has been placed on progesterone. But in reality, one of the three estrogens works together with progesterone in every tissue of a woman’s normal physiology. In vitro studies in human osteoblasts indicate that progesterone is likely working through bone formation pathways, meaning it plays an active role in osteoporosis prevention and bone health. While estrogen is still a dominant focus for osteoporosis in menopausal women, progesterone is emerging as a potentially important hormone partner.
- Testosterone has anabolic (muscle growth and development of muscles) and androgenic (sexual characteristics such as libido, mood, sex drive etc.) effects. These effects are crucial for both men and women (even though men produce significantly more testosterone than women). Human studies show that estrogen is needed for suppressing bone resorption, but both androgen and estrogen are crucial for bone formation.
These inevitable changes in your hormones during menopause can significantly affect your bone health. To combat this bone loss due to hormonal changes, you may need to increase your nutrient intake.
Nutrient Needs Change
As hormone levels diminish during menopause, bone loss may occur and contribute to weak and brittle bones. As discussed, one of the ways in which estrogen supports bone health is by aiding in the absorption of calcium in your intestine. So, ensuring you’re getting an adequate amount of calcium along with the other key vitamins and minerals that assist in its absorption is crucial.
For women 51 years and older, that means getting 1,200 mg of calcium from all sources (food and supplements) each day. Combining calcium with magnesium, vitamin D3, vitamin K2, boron and trace minerals will ensure that your bones are getting all the nutrients they need. But don’t forget about the omega 3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They have been shown to reduce the risk of cognitive decline and cardiovascular disease, and also play a role in protecting your bones. They do this by lessening inflammation. And anything that causes inflammation activates osteoclasts, the cells that break down bone.
As an emphasis on nutrient needs is heightened during menopause, it’s important to ensure you’re getting enough of the right nutrients by supplementing with a clinically supported bone-building supplement and a one-of-a-kind fish oil.
Lack of Sleep and Stress
Insomnia occurs in 40-50% of women during menopause. And problems with a good night’s rest may or may not be connected to mood disorders. Women with insomnia are more likely than others to report tension, depressive symptoms, anxiety, and stress.
A 2005 study published in Clinical Calcium discussed three ways in which stress and bone health are related.
- Stress induces physiological changes leading to osteoporosis. When your body is stressed, it releases a steroid hormone called cortisol. Cortisol indirectly acts on bone by blocking calcium absorption, which decreases bone cell growth. So when you’re stressed for even a short period of time, elevated cortisol may decrease bone mineral density. Stress increases the rate at which your body uses magnesium and your needs for this key bone health mineral.
- Stress induces behavioral distortion of drinking, eating, sleep habits, and exercise that can lead to osteoporosis. Stress can cause insomnia, making it difficult for you to reach the 6-8 hours of sleep you need each night. And for some, it can affect their food, drink, and exercise choices. Harvard Health suggests there is much truth behind “stress eating”. Stress tends to push people towards consuming high-sugar and high-fat foods! Again, this is due to high cortisol levels or a combination of high cortisol and high insulin levels.
- Osteoporosis, on the other hand, can lead to depression, social isolation and stress. If you find yourself in menopausal transition and discover you also have bone loss or osteoporosis…it can be a lot to handle. You may feel stressed, anxious, and lonely. However, know you’re not alone in this journey. There are women just like you currently struggling through similar situations or who have gone through these experiences, and are sharing their success stories with AlgaeCal and its community. We at AlgaeCal encourage the conversation and sharing of experience and information. With this knowledge, you can take your health and life into your own, well-informed hands. If you have any questions or simply want to connect with others like you, comment at the end of this post.
The reality is, approximately 40% of all postmenopausal women will eventually experience a fracture. But, you don’t have to be one of them! Today, women have treatment options to consider.

The Top 8 Natural Menopause Treatment Options
Although menopause is a life stage and not a disease that can be cured, the signs and symptoms affecting quality of life can be tempered in several ways.
The following are natural treatment options, which will vary between each individual and how they want to approach their health.
Bio-identical Hormone Replacement Therapy (BHRT)
BHRT is used to ease menopause symptoms with the goal of raising natural human hormone levels back to normal levels seen in women aged 35 years. The bio-identical human hormones used in BHRT are precisely identical in their biochemical structure to those women naturally produce. So, they function within our bodies like those a woman’s body produces on a daily basis. Therefore, our bodies can’t distinguish these supplemental hormones from those we produce ourselves. When your body sees bio-identical hormones, it welcomes back old friends and knows exactly what to do with them. And, when administered after thorough testing and monitored properly, BHRT hasn’t been found to produce adverse side-effects.
A personal note: Around age 50, I began to notice some changes in my menstrual cycling — more frequent periods and spotting. After running comprehensive hormone tests to get a baseline on my perimenopausal hormone levels, I was prescribed BHRT. I sailed through menopause at age 52 with nary a single symptom.
I’m almost 69 now and have been on BHRT since age 52 with annual testing to ensure my dosages of Bi-est and progesterone are correct for me. My health is excellent in every respect; I feel just as vibrant today as I did at age 35. BHRT is definitely a part of my bone health regimen, but only one part. Like everyone else’s bones, mine won’t maintain themselves healthfully without an optimal supply of all the key nutrients our bones require. Plus I also have a number of genetic susceptibilities for low bone density that BHRT doesn’t address. These, I have identified and corrected through a healthy diet and nutritional supplements, of which the most important for me are AlgaeCal Plus, Strontium Boost, and Triple Power.
For more information on BHRT, read Dr. Jonathan Wright, MD’s most recent book on the topic, Stay Young & Sexy with Bio-identical Hormone Replacement. Don’t be put off by the title. This book provides an easily understandable, and surprisingly entertaining review of virtually all the major studies done over the last 40+ years.
A number of organizations can help you locate a physician knowledgeable about BHRT. All are listed along with their contact information in Stay Young & Sexy with Bio-Identical Hormone Replacement. They include the American College for Advancement in Medicine, the International College of Integrative Medicine, and the American Academy of Environmental Medicine and Women in Balance.
Lifestyle Changes
The choices you make impact the way you feel. For example, smokers have lower levels of estrogen than non-smokers and are more likely to experience hot flashes more frequently than non-smokers. And smoking greatly increases your risk for bone loss and fractures. If you’re currently smoking, please get the help you need to STOP!
Avoid Known Triggers
Hot and spicy foods, caffeine and alcohol may induce hot flashes and contribute to fatigue. If you notice certain foods or drinks trigger episodes, try to avoid them. Caffeine tolerance can vary from woman to woman, so if you know you’re sensitive, react to or are unable to detoxify caffeine efficiently, then it’s something you should consider cutting out. Try decaffeinated coffee instead. You may not even miss the caffeine. Same goes for spicy foods, as they mimic hot flashes by raising your core body temperature. In some cases, they can make you sweat. If you love spicy food, you can still include it in your diet, but do try some spices with less heat as well. You may really enjoy the new flavors and avoid the hot flash effects on your body.
Acupuncture
Acupuncture can be a natural way to ease menopause symptoms. A small study published in 2011 showed that acupuncture was effective in reducing menopausal symptoms, including hot flashes. (That’s the case when compared to “sham treatments”, which are shallow needling procedures that don’t stimulate an acupuncture point.)

Exercise
Exercise can ease menopause symptoms. Multiple studies have shown that working out can reduce hot flashes and improve overall well-being, both mentally and physically. One study from the American College of Sports Medicine found that strength training reduced headaches and hot flashes by 50%! Another study published in The Journal of Physiology measured the characteristic of hot flashes and the impact of exercise with a gym-based program for 16 weeks. While one group undertook this program, the other group made no changes to their daily routine. The exercise group reported reduced symptoms of hot flashes, including less sweating when hot flashes did occur, and decreased arterial pressure.
Vitamin D
You probably know how we derive Vitamin D from the sun. It’s a natural, easy way to get this vital nutrient through our skin. As we age, however, our body becomes less efficient at converting the sun’s rays into the Vitamin D we need.
In fact, a 70-year-old makes 4 times less vitamin D from the sun than a 20-year-old. So it’s important we help our bodies by using dietary supplements. What’s more, vitamin D is a crucial ingredient to healthy bones.
Vitamin D is also linked to a reduced risk of several health issues like: osteoporosis, high blood pressure, heart attacks, asthma, and strokes, among others.
An updated study from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) found Vitamin D gives a big boost to menopausal women as well. ESCEO found having blood levels of 20 ng/mL or less promotes “increased bone turnover, bone loss, and possibly mineralization defects.” That’s in comparison to those with blood levels above that amount.
Instead of guessing how much vitamin D you need, it’s best to be sure and get a vitamin D test.
Either ask your doctor to order this test for you (it should be covered by your insurance) or check out the Vitamin D Council as they have an easy finger-prick mail in test kit you can use. Know your levels, then supplement accordingly!
Magnesium
Another “must” for healthy bones. Magnesium is one of the 13 minerals your bones require to stay strong and functional every day. But do you know the surprising link between magnesium and menopause?
One interesting study came from the Virginia University Health System. It found magnesium supplements can reduce the frequency of hot flashes!
Scientists had 25 women with an average age of 53.5 take magnesium over a 4-week period. They found the majority had a large reduction in hot flashes– from a previous average of 52, down to only 28 per week– for a 41% improvement.
Fatigue, sweating, and distress were also significantly reduced.
And guess what… dark chocolate is a really good source of magnesium! How’s that for a little menopause “secret weapon”?
Calcium
Calcium is the most “common” mineral folks mention when it comes to bone health. And it’s even more critical when we’re talking about menopause.
Because of the drop in estrogen, we also experience a decrease in our ability to absorb, efficiently use and retain calcium during menopause. The loss of estrogen lessens the body’s ability to absorb calcium from our diet. That’s why calcium supplementation (preferably from plant sources) is always advised as we age to ensure optimal amounts of calcium.
And in addition to being a catalyst for strong, healthy bones, calcium can also have positive effects on other unrelated disorders. Things like: high blood pressure, colorectal cancer, obesity, and kidney stone formation.
So together, vitamin D, magnesium, and calcium form the “menopause trifecta” that can help you age gracefully and much more comfortably. They can ease menopause symptoms while also keeping you strong and mobile while they’re at it!
However, supplementing with all three nutrients separately can be irksome. For one, it’s expensive. Two, you must remember to take them and refill your supply– often at different times. And you must ensure you take the right kinds (and amounts) of each!
A Better Bone-Building, Menopause-Soothing Idea
When it comes to the “menopause trifecta” discussed above… there’s an easy solution to these concerns. And it comes in an all-in-one form clinically supported to build bone density at any age (and ease you through menopause).
The best part might be the “secret” ingredient added to the mix. A natural earth element that improves calcium absorption, boosts the activity of your bone-building osteoblasts and lowers the activity of your bone-resorbing osteoclasts, so you become even better at building healthy bone.
Get all the details here… you’ll want to see this regardless of whether you have menopause now!
[ac_banner name=”easemenopause”]
Last Resort: Conventional Menopause Treatment Options
If you’ve exhausted all of your natural treatment options and want to try common mainstream, conventional treatment options, you can consider the following:
- Low-Dose Antidepressants (SSRIs): While estrogen is used for treating night sweats and hot flashes (more on that below), some women are unwilling or unable to use it because of the associated risks. A class of antidepressants called selective serotonin uptake inhibitors (SSRIs) may ease menopausal hot flashes, but these, and other antidepressants cause bone loss. Evidence suggests that SSRIs are among the prescription medications that can increase the risk for osteoporotic fractures. Antidepressants can also lead to migraine headaches, insomnia and an increase in suicidal thinking. All things to consider and weigh up if your only goal is to ease menopause symptoms.
- Vaginal Estrogen: A common menopause symptom is vaginal dryness. To combat this, estrogen can be administered via a vaginal cream, tablet or ring directly into the vagina. This treatment releases a small amount of estrogen that can help ease dryness and discomfort. For a safer, more natural approach, try vaginal water-soluble lubricants, moisturizers or sexual stimulation instead.
- Hormone Replacement Therapy (HRT): HRT is a common treatment to ease menopause symptoms and replaces the hormones that your body no longer makes after menopause with estrogens (derived from pregnant mares’ urine) and drugs called progestins (that were created to mimic some of progesterone’s effects). HRT may consist of Estrogen Therapy (ET) alone or Estrogen Plus Progesterone Therapy (EPT). Estrogen alone can cause cancer in the uterus lining, so women who have had their uterus surgically removed (hysterectomy) may take estrogen alone. EPT is more commonly used by women who still have a uterus.
While HRT has also been shown to increase bone mineral density and slow bone turnover in early and late postmenopausal women, its overall health risks outweigh its benefits. In fact, HRT is associated with a higher incidence of cardiovascular issues (venous thromboembolism, unstable angina) and breast cancer. FDA guidelines emphasize that if you choose to use HRT, it should be used at the lowest effective dose and for the shortest possible time.
Working with an integrative, functional medicine or naturopathic physician who can help you understand and naturally correct the underlying causes of your health issues is your best option.

Recommendations
The really good news is that menopause-associated symptoms are naturally treatable and preventable. It really is possible to sail through menopause with none of them and to embrace this time of your life, instead of enduring it.
Maintaining a healthy lifestyle will ease the transition and circumvent negative, long-term health effects. That means a greater chance of avoiding significant weight gain, heart disease, and bone loss. And to be safe, see your healthcare provider throughout the transition from peri- to postmenopause to continually assess your overall health, including mental, heart and bone health.
I also encourage you to become apart of the AlgaeCal community by participating in conversations on the blog (comment below!) or liking the AlgaeCal Facebook Page, which publishes its own unique content.
By facilitating positive conversation, we can all be the difference in defining a new, natural approach to menopause.





Jean Schuebeler
July 29, 2017 , 9:24 amI had premature menopause from radiation at age 22. I stopped taking HRT when I was 45 years old. I was ahead of my time because I decided that I didn’t want breast cancer and this was before that study came out on HRT/Breast Cancer. I have Osteopenia, which has gotten worse since I decreased Calcium intake and work (waking & standing). Also about 7 years ago I became Heat intolerant (use to love the Heat & humidity). Now just dripping with sweat ! Any idea what this is and what caused it. Thanks