1 in 4 Americans has a secret enemy. And it’s hiding inside them. I’m talking about Non-Alcoholic Fatty Liver Disease (NAFLD). And the worst part? This silent disease doesn’t just wreck your liver. It’s bad news for your bones too!
The name may be a mouthful, but NAFLD simply means excess fat is globbing up your liver. And it’s not the result of one too many cocktail parties – it’s happening to non-drinkers too! The silent epidemic is sweeping across America, set to ensnare even more of us in the coming years [1].
So, what’s causing this fatty liver frenzy? And how can we protect ourselves? Well, the first thing we need to do is understand the vital connection between your liver and your bones.
How Does Your Liver Impact Bone Health?
Your liver is an incredibly hard-working organ that carries out over 500 different functions vital to your body’s health [2]. Among its myriad duties, your liver impacts several aspects of bone health. These include:
Vitamin D activity
Whether you get your vitamin D from sunlight or take it as a supplement, this nutrient requires two steps of conversion before it can become active. First, it must travel to your liver for its initial conversion, and then it’s sent to your kidneys to become active. When your liver isn’t functioning optimally, vitamin D can’t be converted into a form that’s usable by your kidneys, and you end up missing out on this crucial bone-building nutrient [3].
Since vitamin D is essential for calcium absorption, poor liver health directly impacts your bone mineral density.
Detoxification
Your liver is well-known for its detoxification duties. Along with your kidneys, your liver helps relieve the toxic burden your body undergoes each day. And we’re not just talking about the environmental toxins lurking everywhere in our environment, but also the endogenous toxins produced within your body as a result of normal metabolism.
When liver function is suboptimal, toxins build up and create bone-destroying inflammation [4].
And to make matters worse, as your body tries to deal with all of the excess toxins it’s accumulating, it starts to shuttle them into your fat cells for safekeeping. This increases the production and size of fat cells, which can lead to issues like insulin resistance and, you guessed it, fatty liver disease [5].
This means that in an upsetting feedback loop, poor liver health breeds even worse liver health, and your bones take a hit in the process.
Bone-building proteins
Studies show that NAFLD may directly impact the activity of crucial proteins involved in bone metabolism. Specifically, research shows that blood levels of proteins responsible for bone renewal drop (some examples include osteoprotegerin (OPG), osteocalcin, and insulin-like growth factor) while bone-resorbing activity increases [6].
Bile production
Your liver is responsible for producing bile, which helps your body absorb the fat-soluble vitamins A, D, E, and K.
All four of these vitamins play critical roles in bone health, for example:
- Vitamin D is necessary for the absorption of calcium, which is crucial for healthy bone mineral density.
- Vitamin K2 activates the proteins that ferry calcium into our bones and keep it out of soft tissues, like our kidneys, breast, brain, and cardiovascular system [8].
- Vitamin A is needed to balance vitamin D levels and protect against too much calcium absorption. When vitamins A and D are out of balance, it puts us at risk of forming calcium oxalate kidney stones [9].
- Vitamin E protects our cells from inflammation caused by different types of free radicals. Without this essential antioxidant, our risk of excess osteoclast activity (bone resorbing) greatly increases [10].
Therefore, impaired liver function leads to low bile production and potential bone-threatening nutrient deficiencies.
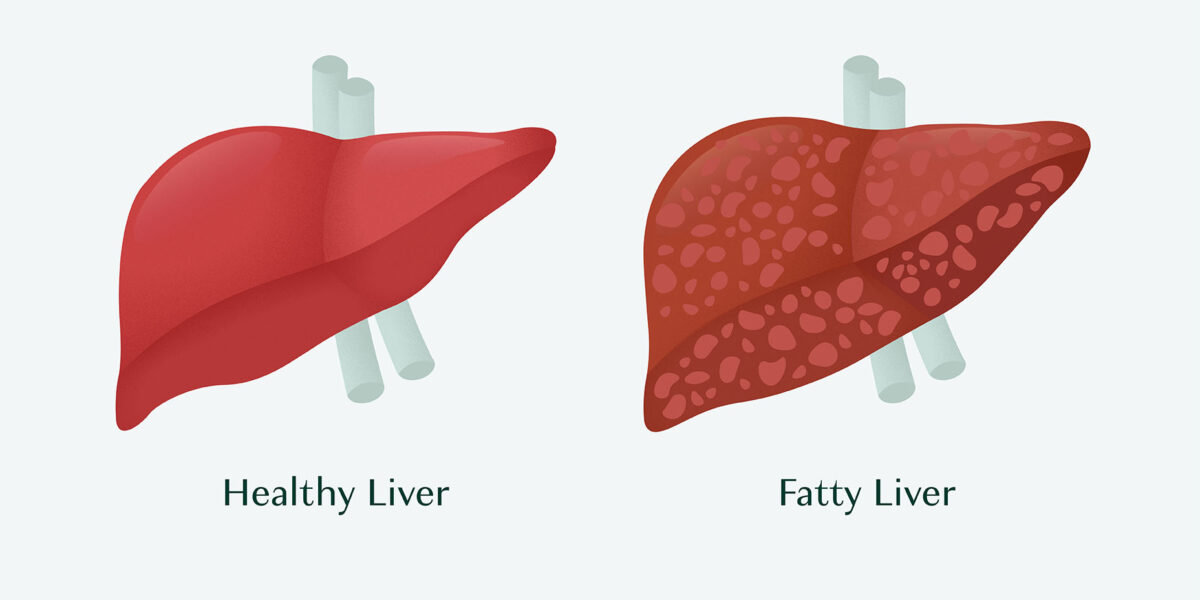
What Causes NAFLD?
Anything that promotes insulin resistance can promote NAFLD. This includes obesity, high blood pressure, high triglyceride levels, low levels of HDL (the “good” cholesterol), or high fasting blood sugar levels [11][12][13].
How does insulin resistance promote NAFLD? Well, far beyond its detoxification duties, your liver plays a central role in processing all the nutrients you take in from your diet.
When glucose levels spike after consumption of refined carbohydrates, your liver converts the excess into triglycerides that get stored in fat cells, like those that accumulate in fat around your waist or on your hips and thighs.
Your liver also converts excess amino acids absorbed from the protein you digest into triglycerides, and these triglycerides are – once again — stored in muscle or fat cells to be converted into glucose for energy when needed.
Normally, very little fat is stored in the liver. Instead, your liver will try to get rid of the excess fat by sending triglycerides out to fat cells for storage. But when your fat cells fill up, they try to send fat back into circulation – where it goes to the liver. The overload of fat and nutrients running through your liver ultimately produces free radicals, which can cause liver damage.
Meanwhile, too much fat in your liver is also associated with too much fat in your bone marrow as well as in your muscles. And in fact, some research suggests that NAFLD may be promoted by sarcopenia when your muscle is replaced by fat [14][15].
Although non-alcoholic fatty liver disease (NAFLD) is usually associated with obesity, individuals who are not overweight can also develop NAFLD. Sadly, what is now being called “Lean NAFLD” or “non-obese NAFLD,” is growing increasingly prevalent. Risk factors for lean NAFLD include fat weight gain even within normal weight limits, insulin resistance, high refined carbohydrate, fructose and high cholesterol intake, increased gut permeability and an altered microbiome – all of which combine to produce sustained inflammation within the liver. Lifestyle modification, including diet and physical activity are the mainstay in treating non-obese NAFLD [16].
Other potential causes of NAFLD include thyroid disease, excessive intake of refined carbohydrates, particularly the high fructose corn syrup used in processed foods (due to the impact on blood sugar), and a sedentary lifestyle.
Five Ways To Protect Your Bones Against NAFLD

#1 Reduce your toxic burden
The number one thing you can do to support your liver is to reduce your overall toxic burden. This includes toxins found around your home and office, as well as in the food you eat. Toxic insults are everywhere these days – personal care products, water, food, cooking appliances; even our clothes can contain environmental toxins [17][18][19].
Your liver will thank you for anything you can do to reduce your toxic burden, but to specifically fend off NAFLD – avoiding sugar is crucial. Particularly high fructose corn syrup (HFCS).
Unfortunately, our food supply is littered with HFCS, so checking labels when you’re at the grocery store is a must. If you think avoiding the obvious culprits like soda and candy is enough, think again. HFCS can be found in all types of packaged foods, including condiments, dressings, snack foods, and even bread.
#2 Consume adequate protein
Conditions like NAFLD are linked to excess body fat and reduced muscle, and when muscle mass is reduced, it puts you at risk for bone diseases like osteoporosis. Therefore, one way to ensure your bones stay healthy and strong is to maintain a diet rich in protein, especially the muscle-building amino acid leucine.
Some leucine-rich foods include [20]:
- Cheese: Gruyere, Emmental, asiago, parmesan, gorgonzola, feta.
- Fish: tuna, salmon, sardines.
- Beans: dried peas, fava beans, tempeh, extra firm tofu, lentils.
- Nuts: pine nuts, almonds, pistachios.
#3 Make movement a priority
Exercise is vital for bone and muscle health for several reasons:
- When you exercise, it inhibits a protein called myostatin. Myostatin not only inhibits muscle cell growth and proliferation, but it also recruits osteoclasts to your bones, which are the cells responsible for breaking down bone [21].
- Exercise increases the release of a hormone-like molecule called Irisin. Irisin lessens insulin resistance, increases your muscles’ use of energy, causes white (inactive) fat to turn into energy-burning brown fat, and triggers the development of osteoblasts (bone-building cells) [22].
- The contraction of your muscles during exercise stimulates the release of the hormone-like compound Beta-aminoisobutyric acid (BAIBA), which protects bone cells from oxidative stress and death. When bone cells die, it stimulates the recruitment of osteoclasts, so in essence, BAIBA slows the process of bone resorption by protecting against an influx of osteoclast activity [23].
- Exercise increases the release of bone-building hormones like osteocalcin, which also plays an important role in our ability to secrete and respond to insulin, improving our ability to use energy instead of overloading the liver [24].
- And, of course, the mechanical pressure of physical activity on bones assists with bone strength and integrity [25].
#4 Ensure you’re getting enough omega-3 fats
Omega-3 fatty acids reduce triglyceride and very low-density lipoprotein (VLDL) levels and are also essential nutrients for optimal bone health. Getting enough omega-3s can help to ensure your bones are strong and healthy while also reducing risk factors for NAFLD [26][27].
That said, it would be very challenging to get enough omega-3s through diet alone, and not all supplements are created equal. That’s why finding a high-quality omega-3 supplement that contains the most bioavailable form of omega-3s from pure and sustainable sources is crucial.
#5 Enjoy your coffee
Although it gets a bad rap at times, studies show that drinking coffee is associated with a lower risk of developing NAFLD, and it’s also good for your bones.
In fact, a recent meta-analysis found that individuals drinking three or more cups of coffee daily had a 27% lower risk of NAFLD. It’s thought that caffeine reduces oxidative stress and liver inflammation, and other substances in coffee, such as cafestol, kahweol, chlorogenic acid, and ferulic acid, are antioxidants that reduce the accumulation of triglyceride and cholesterol in liver cells [28][29].
How Is NAFLD Diagnosed?
NAFLD is usually diagnosed after an unexplained elevation of liver enzymes is seen in blood labs or when liver cells’ infiltration by fat is seen on imaging (e.g., an abdominal ultrasound) [30][31].
In blood tests, elevations in alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase, and bilirubin are biochemical markers of liver injury. Bilirubin also indicates the liver’s ability to detoxify metabolites and transport the resulting compounds into bile.
Tests to visualize the appearance of the liver include ultrasound, computed tomographic (CT) scan, and magnetic resonance imaging (MRI).
You may also receive transient elastography, an ultrasound-based test that measures how stiff the liver is. Or you could receive a liver biopsy, in which a small tissue sample is removed from the liver and checked under a microscope for signs of damage or disease.
Takeaway
NAFLD may be on the rise, but that doesn’t mean you have to fall victim. When you know how to prevent insulin resistance and its accompanying conditions, you can get ahead of complications like NAFLD and potential bone loss.
Incidentally, taking care of your bones and taking care of your liver look very much the same; exercise regularly, eat a whole foods diet, and know how to supplement with high-quality nutrients like omega-3 fatty acids.
To access FREE exercise videos that support your liver and strengthen your bones, join the AlgaeCal Community.
FAQs
What causes fatty liver disease in nonalcoholics?
The most common causes of fatty liver disease in nonalcoholics are insulin resistance, obesity, diabetes, and dyslipidemia. All of which can be traced back to the improper metabolism of nutrients by the liver.
How is NAFLD diagnosed?
The most common way that NAFLD is diagnosed is through the appearance of elevated liver enzymes, alanine aminotransferase (ALT), and aspartate aminotransferase (AST) in a blood test.
Can liver problems cause osteoporosis?
Yes, when the liver isn’t functioning properly, it can interfere with several bone-related processes, including vitamin D regulation, inflammation, nutrient absorption, and the activity of bone-building proteins.
Can the liver recover from NAFLD?
Yes, one of the most effective ways to turn NAFLD around is through sustained weight loss.
References
References
- https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/definition-facts
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/liver-anatomy-and-functions
- Bikle, D. D. (2021). Vitamin D: production, metabolism and mechanisms of action. Endotext [Internet].
- Pizzorno, J., & Pizzorno, L. (2021). Environmental Toxins Are a Major Cause of Bone Loss. Integrative Medicine: A Clinician’s Journal, 20(1), 10.
- La Merrill, M., Emond, C., Kim, M. J., Antignac, J. P., Le Bizec, B., Clément, K., … & Barouki, R. (2013). Toxicological function of adipose tissue: focus on persistent organic pollutants. Environmental health perspectives, 121(2), 162-169.
- Zhao, J., Lei, H., Wang, T., & Xiong, X. (2023). Liver-bone crosstalk in non-alcoholic fatty liver disease: Clinical implications and underlying pathophysiology. Frontiers in Endocrinology, 14.
- Maresz, K. (2015). Proper calcium use: vitamin K2 as a promoter of bone and cardiovascular health. Integrative Medicine: A Clinician’s Journal, 14(1), 34.
- Yee, M. M. F., Chin, K. Y., Ima-Nirwana, S., & Wong, S. K. (2021). Vitamin A and bone health: a review on current evidence. Molecules, 26(6), 1757.
- Wong, S. K., Mohamad, N. V., Ibrahim, N. I., Chin, K. Y., Shuid, A. N., & Ima-Nirwana, S. (2019). The molecular mechanism of vitamin E as a bone-protecting agent: a review on current evidence. International journal of molecular sciences, 20(6), 1453.
- Trojak, A., Waluś-Miarka, M., WoŸniakiewicz, E., Małecki, M. T., & Idzior-Waluś, B. (2013). Nonalcoholic fatty liver disease is associated with low HDL cholesterol and coronary angioplasty in patients with type 2 diabetes. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 19, 1167.
- Tomizawa, M., Kawanabe, Y., Shinozaki, F., Sato, S., Motoyoshi, Y., Sugiyama, T., … & Sueishi, M. (2014). Triglyceride is strongly associated with nonalcoholic fatty liver disease among markers of hyperlipidemia and diabetes. Biomedical reports, 2(5), 633-636.
- Kitade, H., Chen, G., Ni, Y., & Ota, T. (2017). Nonalcoholic fatty liver disease and insulin resistance: new insights and potential new treatments. Nutrients, 9(4), 387.
- Yang, Y. J., & Kim, D. J. (2021). An overview of the molecular mechanisms contributing to musculoskeletal disorders in chronic liver disease: osteoporosis, sarcopenia, and osteoporotic sarcopenia. International Journal of Molecular Sciences, 22(5), 2604.
- Yu, N. Y., Wolfson, T., Middleton, M. S., Hamilton, G., Gamst, A., Angeles, J. E., … & Sirlin, C. B. (2017). Bone marrow fat content is correlated with hepatic fat content in paediatric non-alcoholic fatty liver disease. Clinical radiology, 72(5), 425-e9.
- Albhaisi, S., Chowdhury, A., & Sanyal, A. J. (2019). Non-alcoholic fatty liver disease in lean individuals. JHEP Reports, 1(4), 329-341.
- https://greenbusinessbureau.com/industries/fashion/what-is-toxic-fast-fashion-and-how-does-it-impact-the-environment/
- https://www.ewg.org/the-toxic-twelve-chemicals-and-contaminants-in-cosmetics
- Thompson, L. A., & Darwish, W. S. (2019). Environmental chemical contaminants in food: review of a global problem. Journal of toxicology, 2019.
- Rondanelli, M., Nichetti, M., Peroni, G., Faliva, M. A., Naso, M., Gasparri, C., … & Tartara, A. (2021). Where to find leucine in food and how to feed elderly with sarcopenia in order to counteract loss of muscle mass: Practical advice. Frontiers in Nutrition, 383.
- Zhi, X., Chen, Q., Song, S., Gu, Z., Wei, W., Chen, H., … & Cao, L. (2020). Myostatin promotes osteoclastogenesis by regulating ccdc50 gene expression and RANKL-induced NF-κB and MAPK pathways. Frontiers in Pharmacology, 11, 565163.
- Colaianni, G., Sanesi, L., Storlino, G., Brunetti, G., Colucci, S., & Grano, M. (2019). Irisin and bone: from preclinical studies to the evaluation of its circulating levels in different populations of human subjects. Cells, 8(5), 451.
- Kitase, Y., Vallejo, J. A., Gutheil, W., Vemula, H., Jähn, K., Yi, J., … & Bonewald, L. F. (2018). β-aminoisobutyric acid, l-BAIBA, is a muscle-derived osteocyte survival factor. Cell reports, 22(6), 1531-1544.
- Moser, S. C., & van der Eerden, B. C. (2019). Osteocalcin—A versatile bone-derived hormone. Frontiers in endocrinology, 9, 794.
- Benedetti, M. G., Furlini, G., Zati, A., & Letizia Mauro, G. (2018). The effectiveness of physical exercise on bone density in osteoporotic patients. BioMed research international, 2018.
- Backes, J., Anzalone, D., Hilleman, D., & Catini, J. (2016). The clinical relevance of omega-3 fatty acids in the management of hypertriglyceridemia. Lipids in Health and Disease, 15(1), 1-12.
- Sharma, T., & Mandal, C. C. (2020). Omega‐3 fatty acids in pathological calcification and bone health. Journal of food biochemistry, 44(8), e13333.
- Hayat, U., Siddiqui, A. A., Okut, H., Afroz, S., Tasleem, S., & Haris, A. (2021). The effect of coffee consumption on the non-alcoholic fatty liver disease and liver fibrosis: A meta-analysis of 11 epidemiological studies. Annals of hepatology, 20, 100254.
- Kositamongkol, C., Kanchanasurakit, S., Auttamalang, C., Inchai, N., Kabkaew, T., Kitpark, S., … & Phisalprapa, P. (2021). Coffee consumption and non-alcoholic fatty liver disease: an umbrella review and a systematic review and meta-analysis. Frontiers in Pharmacology, 3442.
- Munteanu, M., Tiniakos, D., Anstee, Q., Charlotte, F., Marchesini, G., Bugianesi, E., … & Mercadier, A. (2016). Diagnostic performance of FibroTest, SteatoTest and ActiTest in patients with NAFLD using the SAF score as histological reference. Alimentary pharmacology & therapeutics, 44(8), 877-889.
- Juo, Y. Y., & Livingston, E. H. (2019). Testing for nonalcoholic fatty liver disease. JAMA, 322(18), 1836-1836.






Karin
August 2, 2023 , 8:23 amThank you, Lara!
I love your articles. Very informative. I’m mostly a plant based eater (wild Alaskan salmon about twice a month). I appreciate it when you cite vegan options.