If you are currently using hormonal contraceptives or have used them in the past, there’s something you need to know. These contraceptives appear to cause greater bone loss after menopause.
Worse yet, recent science is showing that young premenopausal women on these contraceptives are stricken with bone loss during the time in their lives where they should be gaining bone mass!
Bone mass typically increases from birth to about age 35 where it levels off and then starts dropping year after year for the rest of your life. So it’s critical to reach the highest bone mass possible before your mid-thirties. Drugs that not only stop bone mass from increasing but cause an outright bone loss in early life are likely to have devastating effects later in life.
Many hormonal contraceptives cause amenorrhea (a lack of ovulation and menstruation). And all hormonal contraceptives including birth control pills, injections, implants and certain IUDs cause bone loss. This is particularly concerning given that 67% of women who practice contraception are using hormonal methods.
What Are Hormonal Contraceptives And How Do They Cause Bone Loss?
Hormonal contraceptives are devices or medicines that contain the hormones estrogen and progestin. In some cases, they can contain a combination of these hormones and in others, contain only progestin.
The primary use of hormonal contraceptives is for fertility control, however, they can also be taken to reduce ovarian cysts, acne, menstrual cramps, flow and regulate your menstrual cycle.
How do they cause bone loss?
Hormonal contraceptives capable of causing amenorrhea are now being prescribed to girls as young as 14 years of age. Preventing the occurrence of normal menstrual cycles during adolescence results in bone loss during the time in a young woman’s life when major bone accumulation needs to be occurring.
Amenorrhea’s adverse effects on a premenopausal woman’s skeletal mass and strength can even result in severe, premenopausal bone loss, particularly if amenorrhea starts in early adolescence and continues for several years. We fear that losing bone mineral density before menopause may greatly increase risk of severely low bone density in postmenopause.
There are 3 well-known causes of amenorrhea in premenopausal women:
- Rigorous long-term physical training: You may have heard of the female athlete triad, which was first coined in 1992 during a meeting at the American College of Sports Medicine (ACSM). It refers to 3 common problems experienced by female athletes: low energy availability (with or without an eating disorder), menstrual dysfunction and decreased bone mineral density (BMD). Simply put, when you exercise intensely and limit your nutrient intake, you can end up losing your period. As a result, estrogen levels drop and menstruation is no longer triggered.The International Olympic Committee has since updated this term to Relative Energy Deficiency in Sport (RED-S) to encompass both male and female sufferers.
- Anorexia nervosa: Eating disorders such as anorexia nervosa can cause a change in the hormone levels that your body needs to menstruate. In addition, it may cause nutrient deficits, which can be detrimental to the body’s ability to maintain muscle mass, recovery from injury, and build bone.
- The use of contraceptive agents that prevent ovulation: These are present in all forms of hormonal contraceptives (birth control pills, injections, implants, and IUDs). As stated above, preventing the occurrence of normal menstrual cycles during adolescence can lead to less than normal bone density.
Hormonal Contraceptives Do Not Contain Natural Hormones
Hormonal contraceptives do not contain natural human hormones. They contain synthetic hormone-like compounds created to mimic some of the effects of natural human hormones.
Hormonal contraceptives contain progestin, (the progestins are lab-created compounds produce progesterone-like effects), either alone or in combination with a synthetic estrogen-like compound. The two “estrogens” used in hormonal contraceptives in combination with a progestin are EE and mestranol, with EE being much more frequently employed.
But progestins are not progesterone!
The progestin drugs have varying degrees of estrogenic, androgenic, and anti-estrogenic actions, which are thought to be responsible for some of the numerous adverse side effects these drugs produce.
Side Effects Of Hormonal Contraceptives
The first hormonal pill was approved in the 1960s. Since then, oral contraception has been popular worldwide due to its relative ease of taking.
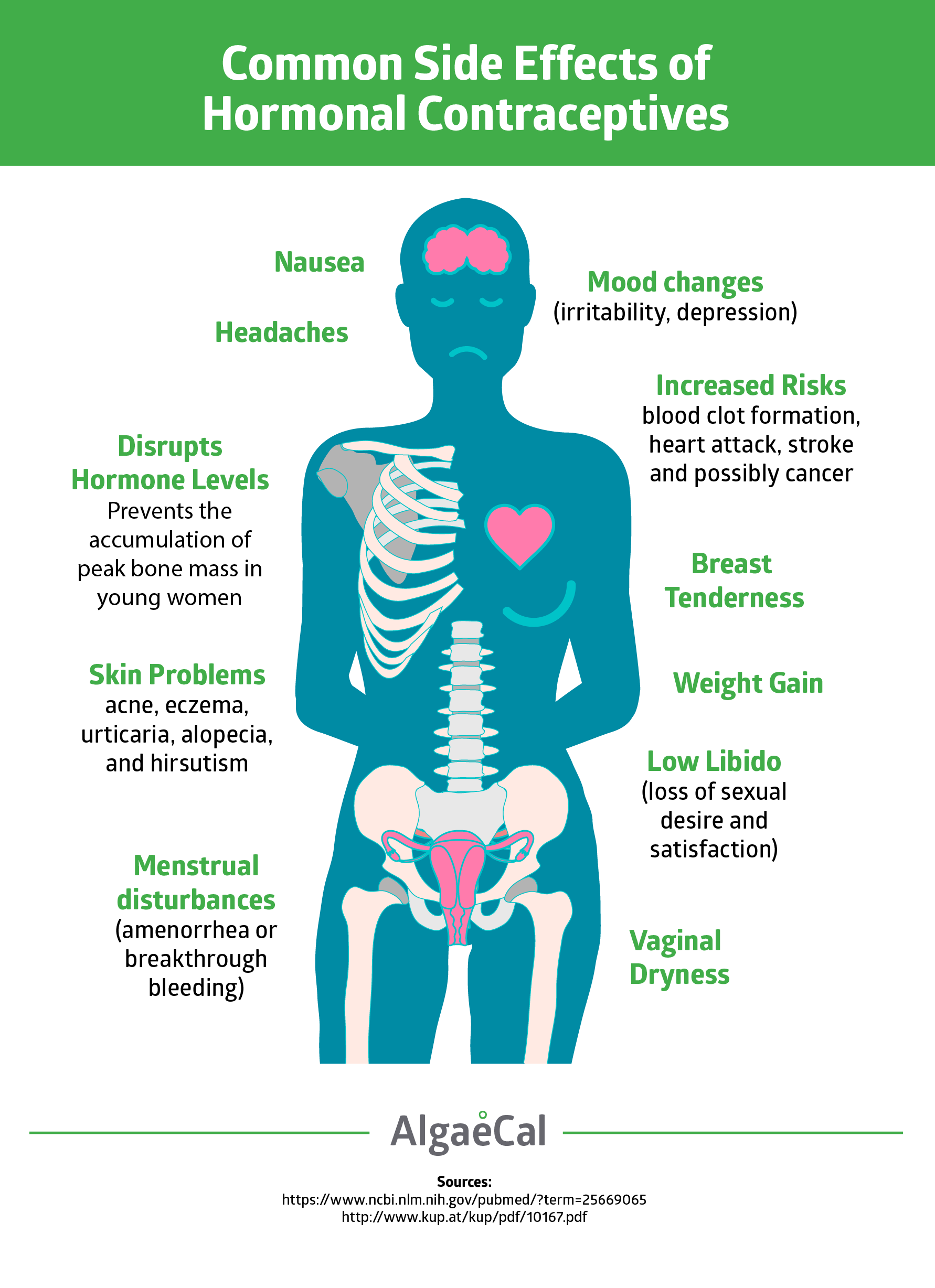
However, in addition to preventing a young woman’s normal accumulation of peak bone mass, hormonal contraceptives have demonstrated the following side-effects:
- Increased risk of blood clot formation, heart attack, stroke and possibly breast cancer
- Menstrual disturbances (amenorrhea or breakthrough bleeding)
- Nausea
- Headaches
- Breast tenderness
- Weight gain
- Mood changes (irritability, depression)
- Vaginal dryness
- Low libido (loss of sexual desire and satisfaction)
- Skin problems (including melasma [dark brown hyperpigmentation], acne, eczema, urticaria [rash/hives]
- Alopecia (hair loss where hair is normally present, e.g., eyebrows, scalp)
- Hirsutism (hair growth where hair is normally not present, e.g., on the face or chest).
[embed_infographic title=”Side Effects of Birth Control” alt=”Side Effects of Birth Contro infographic” src=”algaecal.com/wp-content/uploads/contraceptives-1-1.png”]
Why Do Hormonal Contraceptives Increase Your Risk For All These Side-Effects?
Hormonal contraceptives prevent endocrine glands from functioning properly
The endocrine system is made up of endocrine glands that produce hormones. These glands are the messengers that make sure your body is working as it should! They are chemical substances that release into the bloodstream to direct processes such as sexual development, growth, and metabolism. They also help regulate your emotions.
The major glands of the female endocrine system are the hypothalamus, pituitary, pineal (in your brain), thyroid, parathyroid (in your neck), thymus (between your lungs), adrenals (above your kidneys, pancreas (behind your stomach), and ovaries (in your pelvic region).
When it comes to either a progestin alone or a progestin + “estrogen” contraceptive, it will disrupt the normal functioning of the HPA axis (the hypothalamic-pituitary-ovarian axis, which resides in the center of the brain and is the controlling center for all endocrine functions). Interfering with healthful HPA axis directions can prevent ovulation.
Hormonal contraceptives throw a crank in the gears by suppressing the HPA axis’ secretion of the two hormones that trigger ovulation and a woman’s production of estrogen and progesterone. When a woman takes a hormonal contraceptive, these two hormones — luteinizing hormone [LH] and follicular stimulating hormone [FSH], do not get secreted, and the surge in LH production that should occur mid-menstrual cycle does not occur. All of this is what triggers ovulation, so ovulation doesn’t occur, and no estrogen and progesterone get produced.
Hormonal contraceptives may increase a woman’s risk for severely weak bones in postmenopause
Studies conducted in women in many countries have shown that the use of hormonal contraceptives of all kinds is associated with significant losses in bone mineral density.
Whether such losses increase the risk of fractures later in life is still said to be unclear. Despite the fact that a young woman’s loss rather than gain in bone mineral density (BMD), which studies show happens in the spine, hip and wrist, surely adds to her age-related decline in bone mass, increasing her risk of fracture in these areas.
In hopes of evaluating the research that has been completed on fracture risk related to the use of hormonal contraceptives, a Cochrane Database Systematic Review was conducted. This review, which covered studies of hormonal contraceptives’ effects on fracture risk and/or bone health published through April 2014, identified 19 randomized controlled trials that met its eligibility criteria. Eleven trials compared different combined oral contraceptives (COCs). These COCs contained the estrogen-like compound, EE, plus a progestin, e.g., depot medroxyprogesterone acetate [DMPA], norgestrel, levonorgestrel, northindrone, ethynodiol, and others. Click here for a full list of progestins.
The other 8 trials examined other versions of these contraceptives: injectable forms, implant forms, an IUD, a transdermal patch and a vaginal ring. No trial had fracture as an outcome, instead they measured BMD and various biochemical markers of bone turnover. BMD was measured in 17 of the studies, and 12 trials assessed biochemical markers of bone turnover.
The Cochrane review: all of the trials found hormonal contraceptives, regardless of type, caused loss of BMD.
Despite this, the reviewers said they could not draw strong conclusions because of the mixture of evidence and results. They noted that many of the trials had small numbers of participants; however, they also noted that some of the women in these studies had very large losses of BMD.
Bottom line: Research has found that all types of hormonal contraceptives cause BMD loss. Researchers take the position that it remains to be seen whether they increase a woman’s risk for severely weak bones in postmenopause. To establish a direct link between contraceptives and severely low bone density later in life would require an intervention study where two large groups of women (one group taking the pill and one with placebo) were followed for decades. Don’t hold your breath for that trial to ever happen! They would never get the study approved by the institutional review boards because it’s unethical to give women a placebo birth control pill for starters.
9 Nutrient Deficiencies Caused by “The Pill”
Because so many women use oral contraceptives — with many starting in early adolescence — much research has investigated the physiological changes these drugs produce. These include changes in general health (e.g., fluid retention, irritability, bloating and weight gain) as well as changes in nutritional needs.
Numerous studies have investigated whether women on OCs are at risk of becoming deficient in certain vitamins and minerals. The results seen in these studies caused The World Health Organization (WHO) to issue a report that OCs cause depletions of a number of key nutrients, including key B vitamins (folate, vitamins B2 [riboflavin], B6, and B12), plus vitamin C, vitamin E, and the minerals magnesium, selenium and zinc.
Taking dietary supplements providing these nutrients is essential for women using OCs to prevent vitamin and mineral deficiencies.
Folate
Back in the 1960s, studies have shown that women using OCs not only have lower blood levels of folate, but their folate levels are so low they indicate deficiency of this vitally important nutrient. Furthermore, blood levels of folate continue to decrease with increasing duration of OC use. OCs cause folate deficiency by inhibiting folate’s absorption, increasing its excretion in urine, and increasing the activity of the enzymes that metabolize folates.
Riboflavin (vitamin B2)
Studies dating back to the 1970s have shown riboflavin deficiency is common in women taking OCs. Riboflavin insufficiency leads to degenerative changes in the nervous system, endocrine dysfunction, skin disorders and anemia – and may also be responsible for a commonly reported side effect of OCs – an increase in the frequency, duration and intensity of headaches.
Vitamin B6 (pyridoxine)
If you take OCs and have wondered why you often feel depressed, it may be because B6 deficiency causes deficiency of serotonin, a neurotransmitter that promotes feelings of well-being (and whose production and/or retention is the target of many antidepressant drugs). The most recent studies confirm that women taking OCs should be taking supplemental B6 to avoid deficiency.
Vitamin B12 (cobalamin)
OCs have been shown to prevent B12’s binding to transcobalamin, its carrier in the bloodstream, so this prevents B12’s delivery throughout the body. Impaired B12 status in a pregnant woman greatly increases risk for neural tube defects in her child.
Vitamin C
Vitamin C levels in red blood cells (platelets) and immune cells (leukocytes) are lowered by the use of OCs, specifically those containing estrogen- like compounds. Furthermore, OCs increase oxidative stress (the production of more free radicals than our cells can neutralize), so these drugs increase needs for vitamin C. Vitamin C is required for our production of collagen. Since more than 90% of the protein in the bone matrix is collagen, vitamin C is an essential nutrient for healthy bone.
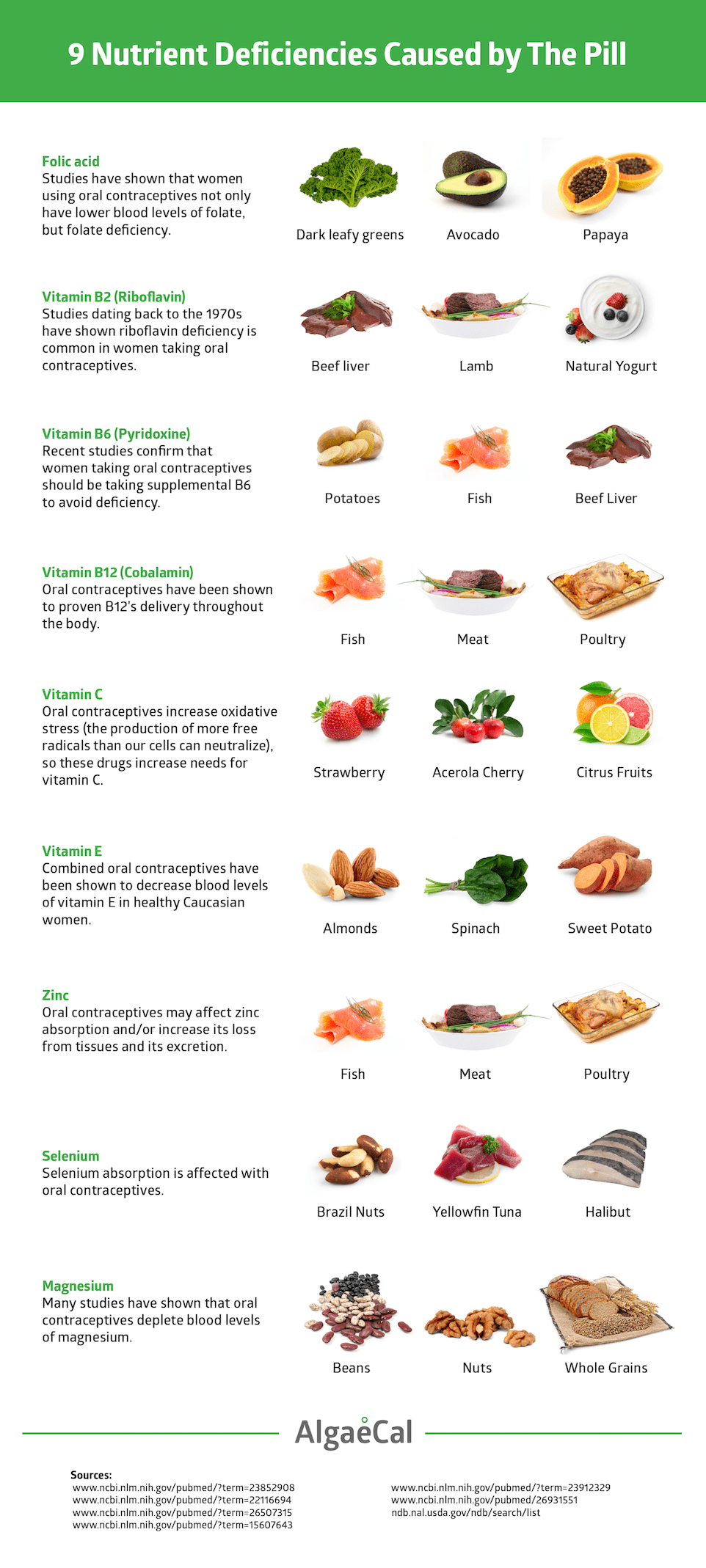
Vitamin E
Combined OCs have been shown to decrease blood levels of vitamin E in healthy Caucasian women, increasing the clotting activity of platelets. Supplementation with vitamin E reversed this adverse effect, leading researchers to speculate that the OC-related increase in heart attack and stroke risk may be due, in part, to these drugs’ lowering of vitamin E levels. Natural vitamin E (mixed tocopherols and tocotrienols, NOT just alpha-tocopherol alone) promotes healthy bones by neutralizing both major types of free radicals (reactive oxygen species and reactive nitrogen species), thus lessening inflammation, and has been shown to increase BMD in middle-aged and elderly human subjects. (Vitamin E supplements that contain only alpha-tocopherol only neutralize reactive oxygen species and actually lower our ability to neutralize reactive nitrogen species, which actually ends up increasing inflammation!)
Zinc
OCs may adversely affect zinc absorption and/or increase its loss from tissues and its excretion. Zinc is essential for healthy immune function. In relation to bone, specifically, zinc inhibits osteoclast production and activity while promoting osteoblast production and activity. Even short-term zinc deficiency decreases bone formation.
Selenium
OCs interfere with selenium absorption. In one study of 200 female students, half of whom had been taking a low-dose triphasic contraceptive medication for a minimum of 3 months, selenium levels were significantly lower in the women taking OCs. (Triphasic OCs contain three different doses of hormones, and the hormone combination changes approximately every 7 days throughout the pill pack. Depending on the pill brand, the amount of estrogen may change as well as the amount of progestin.Selenium also plays a protective role against cancer, particularly breast cancer, probably because of its impact on glutathione production and recycling.
Magnesium
Many studies have shown that OCs deplete blood levels of magnesium, which among numerous other adverse effects, increases risk of blood clot formation, migraine headaches, constipation and muscle cramps. Magnesium is a key player in all living cells: it is required to produce ATP (the energy currency of the body) and is the cofactor in more than 350 enzymes. 60% of the magnesium in the human body is found in bone where magnesium serves as a key constituent of the bone matrix and is required for osteoblast (cell that makes bone) production, development and activity.
Can You Regain BMD Loss Caused by Hormonal Contraceptives?
Yes, you can do much to counteract the bone-destructive effects of hormonal contraceptives!
If you are a premenopausal woman who has been on hormonal contraceptives for several years or even longer, don’t be discouraged. Once hormonal contraceptive use is discontinued, women’s BMD does begin to rebuild.
Several studies have now shown this, including a cross-sectional study that included 135 women, who were divided into three groups:
- Group A, 41 women who were current users of oral contraceptives
- Group B, 51 women who had never used oral contraceptives
- Group C, 41 women who were former users of oral contraceptives.
Each patient completed a questionnaire on demographic parameters, marital state history and contraception history, including duration of use and type of contraceptive pills or other hormonal contraceptive method used. Hip, femur and lumbar spine BMD were measured by DEXA (dual-energy X-ray absorptiometry).
Past users and nonusers showed significantly higher BMD than current users at the spine, femur and forearm. Nonusers had the highest BMD, but even past users had higher BMD levels than current ones. So, this study suggests that bone does begin to rebuild once oral contraceptive use is discontinued.
If you have been using any form of hormonal contraceptive for more than 1 year, consider the following:
- Discuss alternative, safe, forms of contraception with your doctor
- Request a DEXA scan to check your BMD, so you can know now where you stand
- If you cannot switch to one of the many other safe forms of contraception, at least ensure your intake of all the vitamins and minerals the hormonal contraceptive drugs deplete is sufficient to offset the losses they produce
- Provide your bones with optimal amounts of all the key nutrients they must have to successfully rebuild
- You can rely upon AlgaeCal Plus to supply a firm foundation of all essential bone health nutrients in optimal forms and in the dosages shown to be effective in peer-reviewed medical research
- If your DEXA results already indicate low bone density, add Strontium Boost to your daily supplement regimen.
- Scrutinize your diet and lifestyle and minimize all other factors you find that cause bone loss. In essence, this means all factors that promote chronic inflammation.
- Ensure your consumption of anti-inflammatory nutrients, particularly EPA and DHA, the inflammation-busting essential fatty acids, is optimal. Read my other articles on Why Omega 3 Fatty Acids are Crucial for Healthy Bones and How to Determine Your Omega 3 Needs. If your dietary EPA/DHA intake isn’t optimal, consider taking Triple Power Omega 3 Fish Oil.
Putting this all together, you can see that hormonal contraceptives’ adverse effects on bone may be creating an impending tsunami of bone loss. Today’s already frightening statistic of 1 in 3 women over the age of 50 experiencing a fragility fracture does not need to be added to!
If we take action together, we can help prevent much needless harm. Please protect yourself and join me in sharing this information.




Student midwife
June 17, 2018 , 4:12 amHello! I am currently studying to be a midwife (first year), but I have a lot of confusion concerning the effects of estrogen. In college we were taught that estrogen stenghtens bone mass and, therefore, HRT is supposed to also help prevent osteoporosis. If this is the case, then why do combined contraceptive pills cause bone loss?