You’ve begun taking AlgaeCal Plus, Strontium Boost and Triple Power, a fantastic supplement plan to increase bone mineral density and improve overall bone health, but how do you know if it’s working?
Going in for a DEXA scan is the best way to test your bone mineral density, but sometimes you have to wait longer than you’d like for your next scan.
Assessing your bone turnover markers (BTMs) is an excellent way to see what’s happening in your bones in present time. These markers give you information about the activity of your bone-building and bone-resorbing cells in real time, which means that you don’t have to wait to see shifts in their levels.
In this article, we’re going to discuss what bone turnover markers are, when and why you want to check them, and how they can provide you with the information you need to ensure you’re on the right track.
The Bone Remodeling Process
Before we jump into the details of bone turnover markers (BTM), let’s first examine the process of bone remodeling. By understanding how your bones remodel themselves, you’ll better grasp the role of bone turnover markers and why they’re so crucial in helping you assess how well your bones respond to specific protocols.
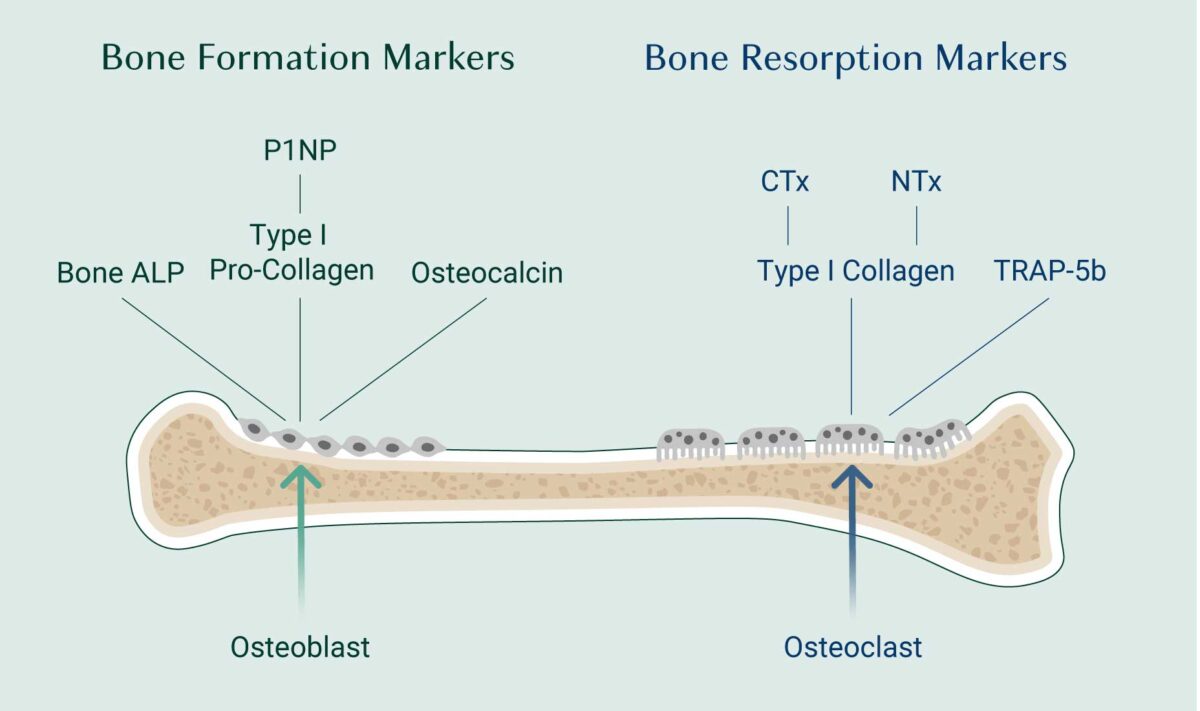
Bone renewal consists of two coupled activities: resorption (or the breakdown) of old or damaged bone carried out by osteoclast cells whose activity releases growth factors and other nutrients that trigger the process new bone formation by osteoblast cells.
During normal healthy bone remodeling, these two processes are tightly coupled with osteoclasts and osteoblasts working together as a team in tiny little multicellular groupings called Basic Multicellular Units or BMUs.
Your BMU crews replace old bone with new bone, ensure your blood levels of calcium remain stable, and your body’s overall pH remains slightly alkaline, and in the process, release compounds that appear in your blood and urine. These are your bone turnover markers.
Therefore, each BTM acts as an indicator of a specific process that’s happening in your bones.
The natural levels of BTMs will shift throughout your life due to changes in bone remodeling that occur with age. Bone turnover markers are highest in growing children, peak during puberty, then tend to remain at relatively low basal levels during adulthood until an increase is observed in postmenopausal women.
For this reason, the ranges for healthy BTMs you want to see on your lab reports are established from research conducted on young women between the ages of 35 and 45 when bone remodeling is low and balanced[1].
How to Get Your Bone Turnover Markers Checked
DEXA scan is the gold standard for testing bone density, so we highly encourage regular DEXA scans to ensure that your bones are healthy and where they need to be. That said, BTMs offer a fantastic adjunct to DEXA as you can assess your BTMs on a more frequent basis.
You can talk to your healthcare provider about ordering regular BTM tests as you work on your treatment plan. It’s always a good idea to test your BTMs close to when you begin on new bone health supplements. This will give you a baseline to work with moving forward so you can compare your results to see how well your bone health plan is working.
Your medical insurance should cover these lab tests. In the U.S., most private insurance plans cover at least one bone turnover marker, as does Medicare under a National Coverage Determination.

Interpreting Your Results
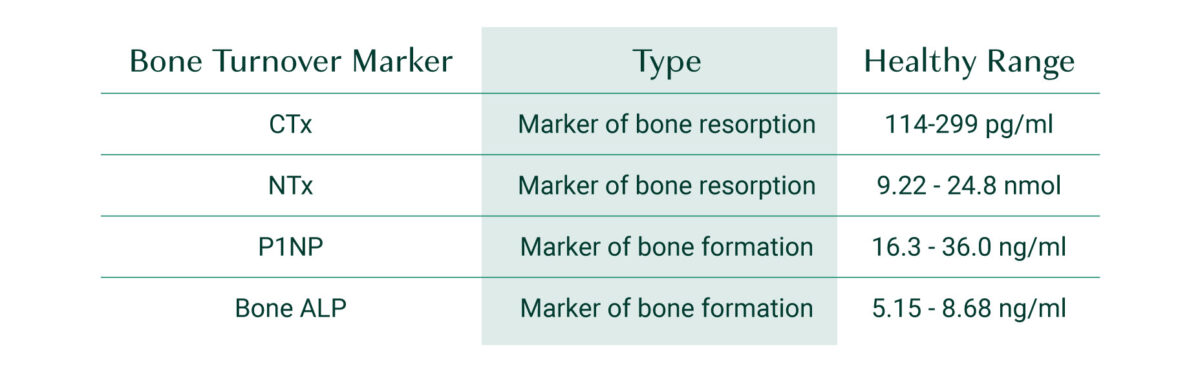
Lab ranges do vary, so it’s best to check your report to see the ranges used by the lab that ran your test, but in general, healthy levels of bone remodeling are indicated by the following ranges[2]:
Markers of Bone Resorption:
- CTx blood levels: 114–299 pg/ml
- Urinary NTx/Creatinine: 9.22–24.8 nmol BCE/mmol creatinine
Markers of Bone Formation:
- P1NP: 16.3–36.0 ng/ml
- Bone ALP: 5.15–8.68 ng/ml
If you find that your BTMs for bone resorption (CTx) are out of range on the high end, it indicates excessive bone turnover. If your BTMs for bone resorption (CTx) are out of range at the low end, it indicates osteoclast activity is suppressed, and remember, bone renewal is coupled. Osteoclast activity is needed to initiate osteoblast activity. If your BTMs for bone formation are out of range on the lower end, it indicates that you’re rebuilding bone too slowly. Ideally, your measurement for P1NP and CTx will both be around mid-range, indicating a healthy balance of bone resorption and bone formation. If your initial levels are out of balance, continue on your bone health plan and then re-test in 3-6 months.
If you see that your levels are moving in the right direction, keep up with your plan.
However, if you notice that your levels are not improving, there are several factors that you can check to see what’s causing either an increase in bone turnover or inadequate new bone formation.
Bone Turnover Markers Explained
As mentioned, while getting a DEXA scan to assess bone mineral density is important, BTMs are helpful for evaluating bone health on a more frequent basis. In fact, within just 12 weeks (3 months), BTMs can tell you if the activities of your osteoclasts and osteoblasts are moving towards—or are already in — a healthy balance.
If you have type 1 or type 2 diabetes, it’s even more crucial that you check BTMs because bone mineral density tends to be less affected by diabetes, but bone health can still suffer. Therefore, DEXA reports often underestimate fracture risk in individuals with diabetes.[1].
Furthermore, if you’re taking anti-resorptive drugs, you retain and accumulate poor-quality bone due to their suppression of osteoclast activity, which you now know is required for osteoblast activity. As a result, you end up with an increase in BMD but also an increasingly greater risk of fracture. Checking your BTMs can provide insight beyond BMD and let you know how healthy your bones are from a fracture-risk standpoint[3].
There are two groups of BTMs: markers of bone resorption that are released by osteoclast activity and markers of bone formation that are released by osteoblast activity. Let’s take a look at each in more detail.
Markers of Bone Resorption
C-terminal telopeptide (CTx)
C-terminal cross-linking telopeptide of type I collagen is currently considered the key marker of bone resorption by the International Osteoporosis Foundation[4].
This BTM is derived from type 1 collagen via the action of osteoclasts (cells that break down bone). Both blood and urine tests will detect CTx, although blood is the superior option for accuracy.
N-terminal telopeptide (NTx)
Much like CTx, NTx is also derived from type 1 collagen via the action of osteoclasts. However, NTx is less accurate than CTx as a bone turnover marker because the test is often run in urine, which is a less reliable sample. If your doctor does run an NTx assessment, it should be run several times with pooled results to give you a more accurate assessment, as NTx levels in urine can fluctuate dramatically[1].
Tartrate-resistant acid phosphatase 5B (TRAP-5B)
In the case of chronic kidney disease, neither CTx nor NTx will be reliable markers for you because these BTMs accumulate when kidney function is compromised.
As an alternative, you can test levels of Tartrate-resistant acid phosphatase 5B. This BTM’s blood levels are not affected by kidney function[5].
Markers of Bone Formation
N-terminal collagen type I extension propeptide (P1NP)
N-terminal collagen type I extension propeptide, which is abbreviated as P1NP, is considered the key marker of bone formation. P1NP is derived from type 1 collagen, which is secreted by osteoblasts (bone-building cells).
There are two forms of P1NP that can be measured; 3-peptide or 1-peptide. When having total P1NP measured, your results will show both forms, but if you have chronic kidney disease (CKD), you’ll want to have “intact” P1NP measured only, which is the 3-peptide form.
This is because a low glomerular filtration rate (GFR) will overestimate P1NP concentrations, giving you false results on your test. With “intact” P1NP, you’ll get a better idea of your true levels[6].
Osteocalcin
Osteocalcin is a calcium-binding enzyme secreted by mature osteoblasts, and it’s the most abundant non-collagen protein found in bone. Blood levels of osteocalcin follow a circadian rhythm, peaking around midnight when bone formation is at its height and then plummeting to its lowest levels around noon.
Because of osteocalcin’s circadian rhythm, if you are going to have your osteocalcin level checked, your blood must be drawn in the morning when you’re fasting.
Bone Alkaline Phosphatase (bone ALP)
Bone-Specific Alkaline Phosphatase (bone ALP) is another enzyme secreted by osteoblasts that plays a vital role in bone mineralization[7].
Alkaline phosphatase can be found throughout your body in different tissues and organs, including your intestines, liver, kidneys, and bones. When you test for bone-specific alkaline phosphatase, it tells you whether your osteoblasts are actively building new bone for you, as this BTM is released in proportion to the activity of bone-building cells.
It should be noted that current lab tests available for bone ALP may include the activity of the form of alkaline phosphatase found in the liver. Therefore, this BTM is not the best choice for you if you have any form of liver disease.
Factors That Can Affect BTMs
BTMs will be affected by any physiological process that’s inhibiting proper bone turnover. Therefore, if you do not see the results you would like to see with your treatment plan, you’ll want to check for secondary causes of osteoporosis, including insufficient weight bearing exercise, insufficient vitamin D, calcium, magnesium or trace minerals, insufficient protein consumption, digestive problems like low stomach acid or dysbiosis that impair your ability to absorb the nutrients your bones need, environmental toxins (like lead, mercury, cadmium, phthalates or pesticides), or conditions like hyperparathyroidism, hypo- or hyperthyroidism, subclinical hypercortisolism, and kidney or liver diseases (e.g., NAFLD, hepatitis)[8][9][10][11].
Furthermore, certain medications such as proton pump inhibitors, glucocorticoid medications, and SSRIs can affect your ability to absorb the nutrients your bones need and/or adversely affect your endocrine system and the activity of your bone building osteoblasts[12][13].
There are also a handful of factors to keep in mind that may impact the reproducibility of your BTM measurements:
- Bone turnover increases in the winter and decreases in the summer. Therefore, if you’re testing throughout the year, you’ll want to keep these fluctuations in mind.
- If you have recently had a fracture, your BTM levels will dramatically increase for at least six months[2].
Glucocorticoid therapy reduces the level of P1NP in a dose-responsive manner. For this reason, P1NP is only helpful in monitoring treatment of glucocorticoid-induced osteoporosis if the glucocorticoid dose is established and remains stable[14].
Takeaway
Now that you know more about how to assess what’s happening with your bone remodeling process, you’ll want to ensure you’re taking the right supplements to support bone health.
First and foremost, to increase bone mineral density, you must have a proper supply of vitamins and minerals like those found in AlgaeCal Plus. If your bone mineral density is already lower than you would like it to be, add Strontium Boost to slow down bone resorption, speed up bone formation, and triple your gains in bone density.
To address oxidative stress that is often at the root of bone loss, consider taking a high-quality omega-3 like Triple Power Omega-3 Fish oil.
Have your BTMs tested, stay committed to your bone health plan and test your BTMs again in 3 to 6 months to make sure everything is moving in the right direction!
FAQs
What is a bone turnover marker test?
A bone turnover marker test assesses biochemical markers for bone resorption and bone formation. This test can give you information about what is happening in your bone remodeling process.
What are biomarkers for bone turnover?
Biomarkers for bone formation include N-terminal collagen type I extension propeptide (P1NP), osteocalcin, and Bone Alkaline Phosphatase (bone ALP). Biomarkers for bone resorption include C-terminal telopeptide (CTx) and N-terminal telopeptide (NTx).
What is CTx bone marker?
C-terminal telopeptide (CTx) is derived from type 1 collagen via the action of osteoclasts; its presence indicates that bone resorption is taking place.
What is a good CTx score?
CTx blood levels should be within the mid-range of 114–299 pg/ml, indicating a healthy balance of bone resorption and bone formation. A CTx out of range on the high end indicates excessive bone turnover. CTx out of range on the low end indicates osteoclast activity is suppressed. Some osteoclast activity is needed to initiate osteoblast activity. If your BTMs for bone formation are out of range on the lower end, it indicates that you’re rebuilding bone too slowly.
What does high bone turnover mean?
High bone turnover is associated with more rapid bone loss than bone formation and can be associated with a range of factors, including age, nutritional status, certain medications, digestive issues, environmental toxins and more. For a full discussion of these issues, please see the book Healthy Bones, Healthy You!.
References
- Greenblatt, Matthew B., Joy N. Tsai, and Marc N. Wein. “Bone turnover markers in the diagnosis and monitoring of metabolic bone disease.” Clinical chemistry 63.2 (2017): 464-474.
- Eastell, Richard, et al. “Diagnosis of endocrine disease: bone turnover markers: are they clinically useful?.” European journal of endocrinology 178.1 (2018): R19-R31.
- Ashrafi, Mehran, et al. “On the effect of antiresorptive drugs on the bone remodeling of the mandible after dental implantation: a mathematical model.” Scientific Reports 11.1 (2021): 1-20.
- Szulc, Pawel. “Bone turnover: Biology and assessment tools.” Best Practice & Research Clinical Endocrinology & Metabolism 32.5 (2018): 725-738.
- Yamada, Shinsuke, et al. “Utility of serum tartrate‐resistant acid phosphatase (TRACP5b) as a bone resorption marker in patients with chronic kidney disease: independence from renal dysfunction.” Clinical endocrinology 69.2 (2008): 189-196.
- Tridimas, Andreas, Anna Milan, and Eileen Marks. “Assessing bone formation in patients with chronic kidney disease using procollagen type I N-terminal propeptide (PINP): The choice of assay makes a difference.” Annals of Clinical Biochemistry 58.5 (2021): 528-536.
- Masrour Roudsari, Jila, and Soleiman Mahjoub. “Quantification and comparison of bone-specific alkaline phosphatase with two methods in normal and paget’s specimens.” Caspian journal of internal medicine 3.3 (2012): 478-483.
- https://www.ncbi.nlm.nih.gov/books/NBK470166/
- Haffner‐Luntzer, Melanie, et al. “Hypochlorhydria‐induced calcium malabsorption does not affect fracture healing but increases post‐traumatic bone loss in the intact skeleton.” Journal of Orthopaedic Research 34.11 (2016): 1914-1921.
- Yatsonsky II, David, et al. “Linkage of microbiota and osteoporosis: a mini literature review.” World Journal of Orthopedics 10.3 (2019): 123.
- Heidelbaugh, Joel J. “Proton pump inhibitors and risk of vitamin and mineral deficiency: evidence and clinical implications.” Therapeutic advances in drug safety 4.3 (2013): 125-133.
- Pizzorno, J., & Pizzorno, L. (2021). Commonly Prescribed and Over-the-Counter Drugs as Secondary Causes of Osteoporosis—Part One. Integrative Medicine: A Clinician’s Journal, 20(2), 8.
- Pizzorno, J., & Pizzorno, L. (2021). Commonly Prescribed and Over-the-Counter Drugs as Secondary Causes of Osteoporosis—Part Two. Integrative Medicine: A Clinician’s Journal, 20(2), 8.
- Eastell, Richard, et al. “Bone formation markers in patients with glucocorticoid-induced osteoporosis treated with teriparatide or alendronate.” Bone 46.4 (2010): 929-934






Wendy Olson
April 15, 2023 , 5:28 amI’m trying to find a good bone Dr. In the 91401 or close to area . Can you help .