The Pathophysiology of Osteoporosis
Pathophysiology of Osteoporosis | Bone Remodeling Process | The Bottom Line | References
Pathophysiology, that’s a mouthful. But what does it mean? Simply, it’s the underlying cause(s) of a health condition — what went wrong, and why.
When it comes to your bones, the pathophysiology of osteoporosis involves many different causes. But they all affect the same thing: the natural balance of how your bones are built up and broken down.
In this article, you’ll discover some of the main culprits behind why this happens. You’ll get to peek inside your bones to see what’s at stake. You’ll also discover a natural way to replace lost bone… and then some!
But first, you need to know about bone remodeling.
What is Bone Remodeling?
Your skeleton isn’t simply a static framework to which your muscles are attached. Your bones are very much alive and active. In fact, 10% of your skeleton is removed and replaced each year(1) — so in 10 years, your entire skeleton will have created itself anew!

That’s called remodeling. Constant, balanced bone remodeling is essential for the maintenance of a healthy skeleton. Just like all cells in your body, your bone cells also get old and worn down, and need replacing. After all, your daily life puts great stress on your bones:
- When you eat, every bite places pressure on your jawbones.
- When you work out, there are micro-damages to your bone. (It’s natural!)
- When you go up or down the stairs, or just walk or jog, you create tiny cracks in your bones.
All this abuse on your bones requires a little TLC. So what determines the rate of bone remodeling? It’s the balance between two cell types, your osteoblasts and osteoclasts.
Osteoblasts: The cells that form new bone.
Osteoclasts: The cells that break down (resorb) old, damaged bone.
These cell types work together to remodel bone and maintain a healthy skeleton.
The Bone Remodeling Process
Remodeling begins when inflammation triggers the osteoclasts to wake up and get to work! Inflammation triggers osteoblasts to produce a protein called the RANK ligand (RANKL). When RANKL activates the RANK receptor on the precursor cells for osteoclasts, these osteoclast-hopefuls get the message that they are to develop into mature osteoclasts and remove worn out, damaged or infected bone.(2)
They start cleaning up areas where there are microfractures in the bone. They release enzymes, which dissolve those areas to remove the old minerals, and different enzymes to digest the organic components (like collagen).
The osteoclasts’ work is normally done in two weeks. And in the following two weeks, the osteoblasts prepare to go to work. Once they arrive on scene, they cover the excavated area with osteoid, a special protein that gets mineralized into new bone.
Finally, after 13 weeks of this action, their job is complete! Just like remodeling a house, it takes a lot longer to rebuild than to break down bone. (Visions of Tom Hanks and Shelly Long in the movie The Money Pit come to mind. Warning: If you are in the middle of remodeling your home, you may find this movie too true to life to be funny.)
The osteoclasts and osteoblasts work together inside a temporary structure called the basic multicellular unit (BMU). Each BMU contains:
- A team of osteoclasts in the front
- A team of osteoblasts in the rear
- A central capillary/blood vessel
- A nerve supply
- Connective tissue
In healthy human adults, 3–4 million BMUs are produced each year with roughly 1 million active at any one moment!
The average lifespan of the osteoclasts and osteoblasts working in tandem inside a healthy BMU is around three to six months. Meanwhile, the lifespan of the whole BMU structure is six to nine months. So, a continuous supply of new osteoclasts and osteoblasts is essential for the BMUs to keep making progress on the bone surface.
Peer Inside Your Bones
There are two basic components to bone, cortical (hard) bone and trabecular (spongy) bone. Think of it like M&M chocolates. The cortical bone is the hard outer shell, while the trabecular bone is the soft inside.
Actually, trabecular bone is more like the inside of an Aero bar. It’s a meshwork of spongy tissue that makes up the inside of our vertebrae (the bones of the spine) and the ends of the long bones (like the hip).
Trabecular bone’s structure is a honeycomb of interconnecting spaces containing bone marrow. This bone marrow is the source of the precursor bone cells that can grow up to become osteoblasts or osteoclasts.
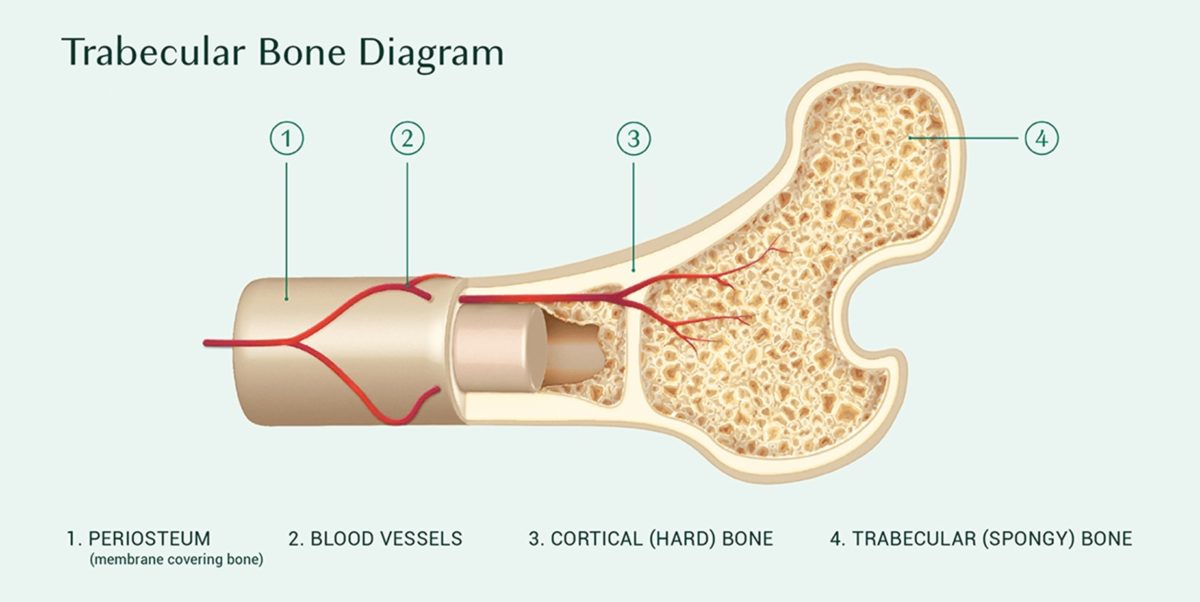
During bone remodeling, the BMU travels through cortical bone, excavating and replacing a tunnel. Then when it reaches the spongy, trabecular bone, the BMU moves across the surface, excavating and replacing a trench.
Our bodies have no trouble producing osteoclasts. But our bone-building osteoblasts are a different story. Let’s look at how osteoporosis occurs and the most common culprits behind it.
What Causes Osteoporosis?

There are two main reasons, and many different culprits behind each:
#1 When the osteoclasts remove bone quicker than the osteoblasts can replace them.
#2 When bone remodeling is inhibited or has ground to a halt.
The key to #1 is inflammation.
Virtually anything that promotes chronic inflammation promotes excessive bone removal.
That’s because inflammation triggers osteoclast production, and we certainly don’t have a deficiency of inflammation! Here are some of the top culprits:
- The Standard American Diet (4)
- Pollutants(5), including pesticides, fluoride, heavy metals(6) (lead, mercury, cadmium, arsenic),
- Endocrine-disrupting chemicals, like BPA and phthalates (7).
There’s also a not-so-obvious part of the Standard American Diet (SAD), which promotes inflammation and that’s the omega 6:omega 3 ratio (8). You know that omega 3 fatty acids are good for you, as they’re powerful antiinflammatories. But you may not know that many omega 6 fatty acids are inflammatory. Some top sources of omega 6s are corn, soybeans, and some oils like canola and soybean.
Unfortunately, much of the SAD is loaded with omega 6s, so the typical omega 6:omega 3 ratio can be upwards of 20:1. Meanwhile, research shows a healthy ratio should be anywhere around 1:1 to 4:1.
Now, cause #2 of osteoporosis (when bone remodeling is inhibited or has ground to a halt) is where things get tricky.
When osteoclast activity is prevented, old and damaged bone accumulates. And that gradually turns the bone fragile, increasing risk of fracture. On the other hand, when osteoblasts are deprived of the nutrients they need to lay down new bone, they won’t strengthen your bones either.
Bone remodeling is also blocked by antiresorptive drugs and monoclonal antibody drugs.
The antiresorptive drugs(9) poison osteoclasts, while monoclonal antibody drugs used to treat osteoporosis prevent them from even developing. Both types of drugs inhibit new bone formation because old or damaged bone must be removed before new bone can be laid down.
Now, it’s not just what we’re putting in our bones that affects their density. It’s what we aren’t putting in them!
Just as you can’t make a cake without eggs, flour, butter, and more, you can’t build bone without calcium, vitamin D, vitamin K2, magnesium, boron, and a number of other trace minerals. And you need proper amounts of protein and collagen, too.
Bones are living tissue. And just like any other tissue in your body, they contain more than one ingredient.
The Bottom Line
The pathophysiology of osteoporosis stems from an imbalance between bone resorption by osteoclasts and bone formation by osteoblasts. Unfortunately, many factors in our modern lifestyles can disrupt this crucial balance. One of the top culprits is inflammation, which triggers osteoclasts to be chronically activated or blocks the osteoblasts’ ability to lay down new bone.
Plus, if osteoblasts don’t receive the nutrition they need, that can also upset bone remodeling.
The solution is not to prevent all osteoclast activity, but to restore balanced bone remodeling. This is done by:
- Identify your inflammation triggers that promote excessive osteoclast activation. Then, control or eliminate them.
- Ensure your osteoblasts receive the proper nutrition they need to lay down new bone at a healthy rate.
References
- Wheeless C. Bone remodeling. Wheeless’ Textbook of Orthopaedics. Duke University. http://www.wheelessonline.com/ortho/bone_remodeling.
- Armour KJ, Armour KE. Inflammation-induced osteoporosis. The IMO model. Methods Mol Med. 2003;80:353-60. PMID: 12728730
- Das S, Crockett JC. Osteoporosis – a current view of pharmacological prevention and treatment. Drug Des Devel Ther. 2013 May 31;7:435-48. doi: 10.2147/DDDT.S31504. Print 2013. PMID: 23807838
- Ilich JZ, Kelly OJ, Kim Y, Spicer MT. Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Arh Hig Rada Toksikol. 2014 Jun;65(2):139-48. doi: 10.2478/10004-1254-65-2014-2541. PMID: 24945416
- Chang KH, Chang MY, Muo CH, et al. Exposure to Air pollution Increases the Risk of Osteoporosis: A Nationwide Longitudinal Study. Medicine (Baltimore). 2015 May;94(17):e733. doi: 10.1097/MD.0000000000000733. PMID: 25929905
- Jalil C, Kazemi M, Taheri E, et al. Exposure to heavy metals and the risk of osteopenia or osteoporosis: a systematic review and meta-analysis. Osteoporosis International. 2020 May. 31, 1671–1682
- Vitu J, Kolatorova L, Franekova L, et al. Endocrine Disruptors of the Bisphenol and Paraben Families and Bone Metabolism. Physiol. Res. 67 (Suppl. 3): S455-S464, 2018
- Simopoulos A. The omega 6/omega 3 fatty acid ratio: health implications. OCL 2010 ; 17(5) : 267–2759.
- Ganesan K, Goyal A, Roane D. Bisphosphonate. [Updated 2021 Jul 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.



Joy Noel
May 6, 2022 , 8:01 pmOsteoporosis sneaks up on you! At 40, healthy and fit, it wasn’t even a consideration. Here, at 70, the bone density comes back a -3.0! Start early, people! Thank goodness there is hope. I’ll be back to report on my AlgaeCal experience!