JAMA Study Confirms:
Inadequate Vitamin D + Below RDI Calcium Intake + No Vitamin K2 = No Help for Postmenopausal Women’s Bones
That’s what the study just published August 3, 2015 in the Journal of the American Medical Association (JAMA) tells us.
Medline, had a different take on the JAMA study’s results. They lead with a headline that informs us: “No Bone Benefit Seen for High Vit D Doses After Menopause”
You’re sure to see variations on the Medline theme in the news. Every major media outlet is telling us that we should forget about vitamin D being of any use to postmenopausal women who want to have healthy bones.
This is not only misleading, but puts people who don’t have the real facts in danger.
You see, there will be people who read these headlines and misleading articles and quit taking vitamin D.
But we MUST have vitamin D to build healthy bone! Not enough vitamin D will put you at an increased risk of osteoporosis.
Just read the full JAMA article. You won’t be fooled (although you may be angered) by the media distortions.
I’m here to provide you with the actual data from the JAMA study – and the facts speak eloquently for themselves – this study was designed to fail.
The JAMA article is titled, “Treatment of Vitamin D Insufficiency in Postmenopausal Women A Randomized Clinical Trial”
What did the researchers actually do?
They took 230 postmenopausal women 75 years or younger. These women were frankly vitamin D deficient but did not have osteoporosis. At the start of the study, the women’s vitamin D levels were measured by their blood levels of 25(OH)D (the form in which vitamin D circulates in the bloodstream).
They were so low that they ranged from a very scary 14 ng/mL to a still-deficient level of 27 ng/mL.
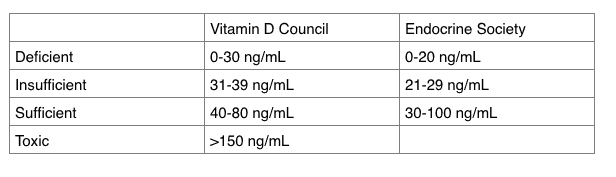
To put these numbers into perspective, the guidelines for vitamin D sufficiency from the Vitamin D Council and the Endocrine Society, two leading authorities in the field, clearly showed these women lacked sufficient vitamin D.
The Vitamin D Council suggests that the ideal level to aim for is 50 ng/mL. This is why the Vitamin D Council recommends that adults take 5,000 IU/day of a vitamin D3 supplement to reach and stay at this level.
The Endocrine Society recommends taking a vitamin D3 supplement of around 2,000 IU/day to reach and stay above a level of 30 ng/mL, which it considers the very lowest level of vitamin D sufficiency.
The postmenopausal women in this study were divided into 3 groups.
- Group one received placebo supplements and a placebo “vitamin D” injection twice a month.
- Group two received supplements providing just 800 IU of vitamin D3 every day and a placebo “vitamin D” injection twice a month.
- Group three received daily supplements that were all placebos except for twice a month, when they were given an injection containing 50,000 IU of vitamin D3.
The groups received their supplements for one year. After the year was up:
- Group one had an average 25(OH)D level of just 19 ng/mL (deficient).
- Group two, which was given 800 IU of vitamin D each day, had an average 25(OH)D level was 28ng/mL–still deficient.
- Group three, which was given 50,000 IU of D3 twice a month, had 25(OH)D levels that averaged 56ng/mL. It’s important to note that 5 of the 79 women in this group (6.3% of them) required additional vitamin D to even reach and maintain 25(OH)D levels of 30 ng/mL. And remember, 30 ng/mL indicates vitamin D deficiency according to the Vitamin D Council and borderline insufficiency according to the Endocrine Society.
So even in the “high-dose” group, a number of the women remained vitamin D deficient/insufficient.
So, the takeaway here is that it’s not surprising that 50,000 IU of vitamin D twice per month is less likely to improve the level of vitamin D (25(OH)D) circulating in your bloodstream than taking 2,000 -5,000 IU of vitamin D3 each day.
Particularly if you are obese, which 75% of the women in the “high-dose” group were according to the information provided in the JAMA article.
A BMI greater than 30 is considered obese; the average BMI of the women in “high-dose” group was 30.7.
The response to vitamin D is dependent on body weight.
Obese women require significantly more vitamin D to increase their blood levels of 25(OH)D than do women with a normal BMI.
What did the researchers have to do with these “high-dose” women whose 25(OH)D levels didn’t even get up to 30 ng/mL when they were given an injection of vitamin D3 containing 50,000 IU twice a month?
A quote from the JAMA article is in order here: “For example, a woman whose 25(OH)D level was 25 ng/mL received 50,000 IU/d of cholecalciferol [vitamin D3] for 7 days then 50,000 IU once weekly to achieve and maintain repletion [which in this study was defined as just 30 ng/mL – and this is NOT repletion!].”
In other words, they had to give these women 50,000 IU every day for a week and then 50,000 IU once a week after that to just get their vitamin D levels up to borderline insufficiency.
Remember that obesity = a BMI of 30 or more. Not only was the average BMI of the women in the “high-dose” vitamin D group 30.7, but the average BMI of the women in the low dose vitamin D group (800 IU/day of vitamin D3) was even higher: 31.2.
It’s obvious that these obese women who were only getting 800 IU/day were not getting anywhere near an amount of vitamin D3 sufficient to help them reach levels of vitamin D3 that could help them absorb more calcium.
In addition, the JAMA article reporting on this study does not tell us how many women in the high-dose group continued to have vitamin D levels 30 ng/mL or below – all we are given is the “average” 25(OH)D level of the entire group.
And this means that a few of the women might have had a very good response while most of the others had a lousy response. When you add all the responses together and divide by the number of women in the group, you get the average.
What you don’t get is what happened to the real people, the real individual women in this study. And the mythical “average human being” does not exist. YOU are not average. YOU are unique, and like some of the women in the high dose group in this study, YOU may require more vitamin D3 than “average.”
One fact that is resoundingly clear from the data collected in this study is that not a single one of the women given just 800 IU/day attained anywhere close to optimal levels of vitamin D. Two points to be made here:
- How much vitamin D3 do you want for yourself? Enough to put you on the borderline of being insufficient/frankly deficient? Or enough to put you at the level where vitamin D is optimally able to help you absorb the calcium your bones must have to stay healthy? Personally, I vote for optimal!
- Since none – not a single one — of the women in this study got anywhere near optimal blood levels of vitamin D by taking an 800 IU/day dose of vitamin D3, we can be pretty sure that this very low dose won’t help any of us either.
Now, how does not getting enough vitamin D3 impact your bones?
Without adequate vitamin D, only 10–15% of dietary (or supplemental calcium) consumed is absorbed.
So, how much calcium were the women in this study getting?
Another fact that isn’t being highlighted in the media reports on this study is how little calcium these postmenopausal vitamin D-deficient women were consuming.
A key “objective” of this study was to see if giving these women low doses of vitamin D – or a high dose as an injection twice a month – would help them to absorb more calcium.
Even if your intake of vitamin D is adequate – which it was not in this study. (Because for most of us adequate vitamin D intake means you are getting between 2,000 and 5,000 IU of vitamin D3 per day). It’s impossible to do a great job of absorbing calcium if you are not consuming calcium in adequate amounts.
The postmenopausal women in this study were counseled to consume 600 to 1400 mg/day of calcium. Based on the information provided in the JAMA article, calcium intake in 75% of study participants was well below 1,200 mg per day – and 1,200 mg is the amount of calcium recommended per day for postmenopausal women.
In fact, as much as 1,500 mg of calcium per day is recommended for postmenopausal women not on hormone replacement, which includes all the women who participated in this study. Women taking estrogen replacement were excluded from participating in this study.
In group two, (the women given 800 IU/day of vitamin D3) calcium intake averaged 961 mg/d, with some participants getting as little as 699 mg/day.
In group three, (the women given 50,000 IU injections of vitamin D3 twice a month) calcium intake averaged 962 mg/day, and some of these women were getting as little as 739 mg /day. Again, well below the RDI for calcium intake in postmenopausal women.
Vitamin K2 – Vitamin D’s Essential Partner that Delivers Calcium to Our Bones – Not Even Mentioned in the JAMA study
Vitamin D – in adequate amounts – increases our ability to absorb calcium – a lot. As already noted, without adequate vitamin D, only 10–15% of dietary (or supplemental calcium) consumed is absorbed. Vitamin D also increases the body’s production of the vitamin K-dependent proteins. Why? Because vitamin D only helps us absorb calcium; it does nothing to regulate where that calcium goes inside our bodies. That’s vitamin K2’s job.
We want the calcium vitamin D helps us absorb to go into our bones – and not into our arteries, kidneys, breasts or brains. Putting calcium into our bones, and keeping it out of our arteries, etc., is the job of proteins that can’t function without vitamin K2 as their co-factor.
The two critical vitamin K-dependent proteins that regulate what happens to the calcium vitamin D helps us absorb are called osteocalcin, which puts calcium into our bones where we want it, and matrix Gla protein, which keeps calcium out of our arteries, and other soft tissues, where we don’t want it!
Even if the women in the JAMA study had been given the RDI (recommended daily intake) of calcium along with enough vitamin D3 to make a difference in their ability to absorb calcium, this still would not have ensured that the calcium they were absorbing was going into their bones. For that, they needed vitamin K2 – which wasn’t even considered as important enough to mention in this study.
Very Little Vitamin K2 in the Food Supply – To Put Calcium into Bone, A Supplement is Needed
It’s close to impossible, unless you eat a Japanese fermented soybean product called natto regularly, to get sufficient vitamin K2 from your diet. If you have a copy of Your Bones, 2nd edition, you’ll find a chart showing the Food Sources of Vitamin K2 on page 183.
Bottom line:
If you require 2,000 IU/day to get your blood levels of vitamin D up and out of the deficiency range (30 ng/mL or lower), you will need at least 100 micrograms of the MK-7 form of K2 each day to fully activate the vitamin K-dependent proteins that put calcium into your bones and keep it from depositing in your arteries.
In Japan, people who eat natto regularly are getting 300-400 micrograms or even more of MK-7 with each serving. In the Netherlands, where certain European high fat cheeses from pastured animals are regularly consumed (e.g., Swiss Emmenthaler, Norwegian Jarlsberg), average daily intake of MK-7 is still just 45 micrograms a day. If you can find these full fat European cheeses, you would have to consume at least 3 ounces daily to ensure getting 40 micrograms of MK-7. The typical Western diet contains far less than 40 micrograms of MK-7 per day. In the United States, very little vitamin K2 is present in the food supply, so little that food sources of vitamin K2 have not even been systematically assessed.
No vitamin D from the sun allowed for the postmenopausal women in the JAMA study
 The JAMA study took place in Madison, Wisconsin. This is an area whose northern latitude renders vitamin D production from sun exposure virtually impossible during a good part of the fall and all through the winter.
The JAMA study took place in Madison, Wisconsin. This is an area whose northern latitude renders vitamin D production from sun exposure virtually impossible during a good part of the fall and all through the winter.
But, just in case some of these women might have been able to produce a bit of vitamin D naturally by being outside in the sunshine during the spring and summer months, the researchers dispensed Total Block sunscreen to participants, who were told to use it between April and October.
While I understand that the scientists conducting this research wanted to only look at the effects of supplemental vitamin D on calcium absorption, I am distressed by what was done to the postmenopausal women who volunteered to participate.
These women were given an inadequate amount of vitamin D, despite their known severely deficient vitamin D status. No calcium supplement was provided, despite the finding that calcium intake in the majority of participants was below the 1,200 mg per day recommended for postmenopausal women. And no information about the necessity of taking vitamin K2 along with vitamin D3 to ensure the calcium they did manage to absorb was used to produce healthy bones and not deposited in their arteries.
Well, now that you know the facts about how this study was conducted, you won’t be surprised to read that – to quote the researchers —
“Though the vitamin D increased calcium absorption in the arm with the highest doses after one year of supplementation, the effect was small and had no clinical bearing.”
I certainly agree with that.
Calcium absorption increased by a meaningless 1% in the high-dosage (50,000 IU by injection twice a month) group, while decreasing 2% in the low-dosage (800 IU/day) arm and decreasing 1.3% in the women given a placebo.
Furthermore, “There were no changes between the three groups in spine, mean total-hip, mean femoral neck, or total-body bone mineral density.” Well, duh. Inadequate vitamin D + inadequate calcium + no vitamin K2 does NOT build bones!
The study’s authors concluded: “Study results do not justify the common and frequently touted practice of administering high-dose cholecalciferol [vitamin D] to older adults to maintain serum 25(OH)D levels of 30 ng/mL or greater.”
REALITY CHECK: The results of this study actually show that giving obese postmenopausal women 800 IU of vitamin D3 per day or a 50,000 IU injection twice a month combined with below RDI intake of calcium and without supplemental vitamin K2 does nothing for their bones.
What can YOU learn from this study that can help YOU to have healthier bones?
If you have not already done so, get your levels of 25(OH)D tested. The Vitamin D Council will now send you a test kit in the mail. It’s easy and very accurate– a tiny finger prick is all that’s needed to get a drop of blood for this test – and then you just pop it back in the mail.
AlgaeCal Plus will provide you with 1,600 IU of vitamin D3, every day.
Once you know what your blood levels of vitamin D are, you can determine if you are taking enough vitamin D3 to keep your levels in the optimal (50-80 ng/mL) range. If not, you will want to increase your intake of vitamin D3 – the Vitamin D Council recommends increasing to 5,000 IU/day for 3 months and then retesting.
Our blood levels of vitamin D tend to be a bit higher in the spring and summer when we can enjoy being outside in the sunshine (without Total Sunblock on our skin!). In the winter, however, we often need a bit more supplemental vitamin D3. Make sure you test your vitamin D levels in winter as well as summer to be sure you are maintaining a healthy supply of vitamin D all year round.
Ensure you are getting at least 1,200 mg of calcium every day from your diet and supplements.
For optimal bone health, postmenopausal women not on hormone replacement may need as much as 1,500 mg of calcium daily.
AlgaeCal Plus will give you 4 different kinds of plant-derived calcium supplying 720 mg of calcium daily; the rest can easily be provided by your diet.
Many delicious, healthy, inexpensive foods – including yogurt, cheeses, spinach, almonds, tofu, canned salmon, sardines, and many more — contain calcium. If you have a copy of Your Bones, 2nd edition, a full listing calcium-rich foods and how much is in a normal serving can be found on p. 87.
Don’t forget about vitamin K2!
You need at least 100 micrograms of the MK-7 form of K2 daily.
If you’re taking AlgaeCal Plus, 100 micrograms of K2 is already provided for you.
Sources:
Hansen KE, Johnson R, Chambers KR, et al. Treatment of Vitamin D Insufficiency in Postmenopausal Women: A Randomized Clinical Trial. JAMA Intern Med. Published online August 03, 2015. doi:10.1001/jamainternmed.2015.3874.
Gallagher JC, Yalamanchili V, Smith LM.The effect of vitamin D supplementation on serum 25(OH)D in thin and obese women. J Steroid Biochem Mol Biol. 2013 Jul;136:195-200. doi:10.1016/j.jsbmb.2012.12.003. Epub 2012 Dec 11. PMID: 23246640
Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30. doi: 10.1210/jc.2011-0385. Epub 2011 Jun 6. PMID: 21646368
Booth SL.Vitamin K: food composition and dietary intakes. Food Nutr Res. 2012;56. doi: 10.3402/fnr.v56i0.5505. Epub 2012 Apr 2. PMID: 22489217
Calcium photo via Pixabay






Dean Neuls
August 13, 2015 , 8:55 amGreat article Lara! Your expertise in this area really helps guide us through the maze of studies.