What exactly does healthy estrogen production look like after menopause?
This hormone continues to play an essential role in your body long after menopause, which is why keeping an eye on your estrogen levels post menopause is just as important as during the menopausal transition.
In this article, I’ll walk you through the three different forms of estrogen, how estrogen impacts bone mineral density, and the best way to check your estrogen levels.
The Three Different Forms of Estrogen
While estrogen is often used as a catch-all term, there are actually three different forms of estrogen to be aware of. Each form plays unique roles in your body and is more or less active at different times in your life, particularly during and after the reproductive period.
Estrone
Estrone (E1) is the primary form of estrogen produced after menopause, primarily synthesized in fat tissue. Estrone is a major source of estradiol formation in our bones and plays a vital role in our ability to maintain healthy bones, especially in older people.
Estrone is also converted into other metabolites, some protecting against breast and prostate cancers and others that can increase risk.
Estrone’s potentially inflammatory metabolites, which can increase the risk of cancer if produced in large amounts, are 4-hydroxyestrone (4-OH estrone) and 16α-OH estrone. That said, small amounts of 16α-OH estrone are essential for bone health as this estrone metabolite has a potent estrogenic effect and strongly induces osteoblast (bone-building) formation and activity [1].
Therefore, the production of 16α-OH estrone is crucial not only for cancer prevention but also for maintaining healthy bones in women as well as men.
Estrone’s protective metabolites include 2-hydroxyestrone (2-OH estrone), 2-methoxyestrone (2-CH3O-estrone), and estriol (E3).
Estradiol
Estradiol (E2) is the most active form of estrogen and is the primary form of circulating estrogen during our reproductive years. We produce estradiol from estrone and also from testosterone.
In your body, estradiol will either be circulating in your bloodstream, converted to estrone, or metabolized into one of its two protective derivatives; 2-OH estradiol and 2-methoxyestradiol.
Estriol
Estriol (E3) is most active during pregnancy and is derived from estrone that has been metabolized into16α-OH estrone (the metabolite that impacts bone health and cancer) but then quickly converted into estriol.
Estriol is the weakest estrogen. It slows down new cell production, imparting an antiproliferative effect in estrogen-sensitive tissues (like the breast, cervix, uterus, and prostate).
Estriol also turns down inflammation and the activation of pro-inflammatory molecules in various pathways and specifically lessens activation of a key pathway of osteoclast (bone resorption) activation [2][3][4].
Estrogen’s Effect on Bone Density
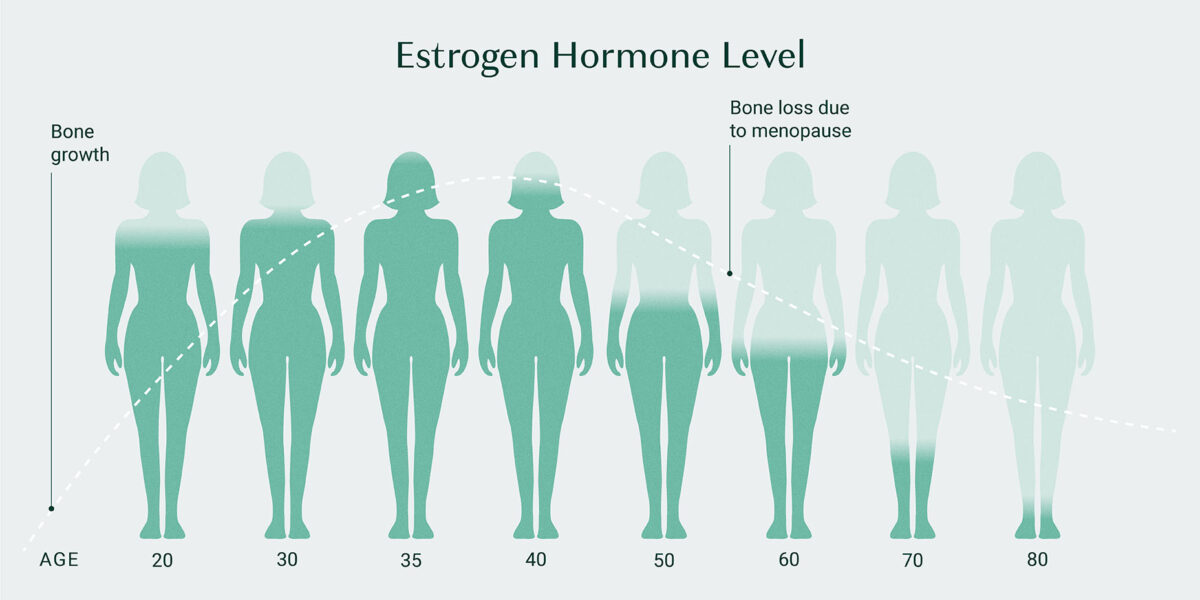
Low estrogen levels are directly associated with bone loss due to the vital roles estrogen plays in bone metabolism. This is why so many women begin to experience bone mineral density (BMD) issues around their menopausal years, as estrogen naturally begins to decline.
This is also why postmenopausal treatment with estrogen is shown to result in significantly reduced markers of bone resorption [5].
But how exactly does estrogen impact bone turnover?
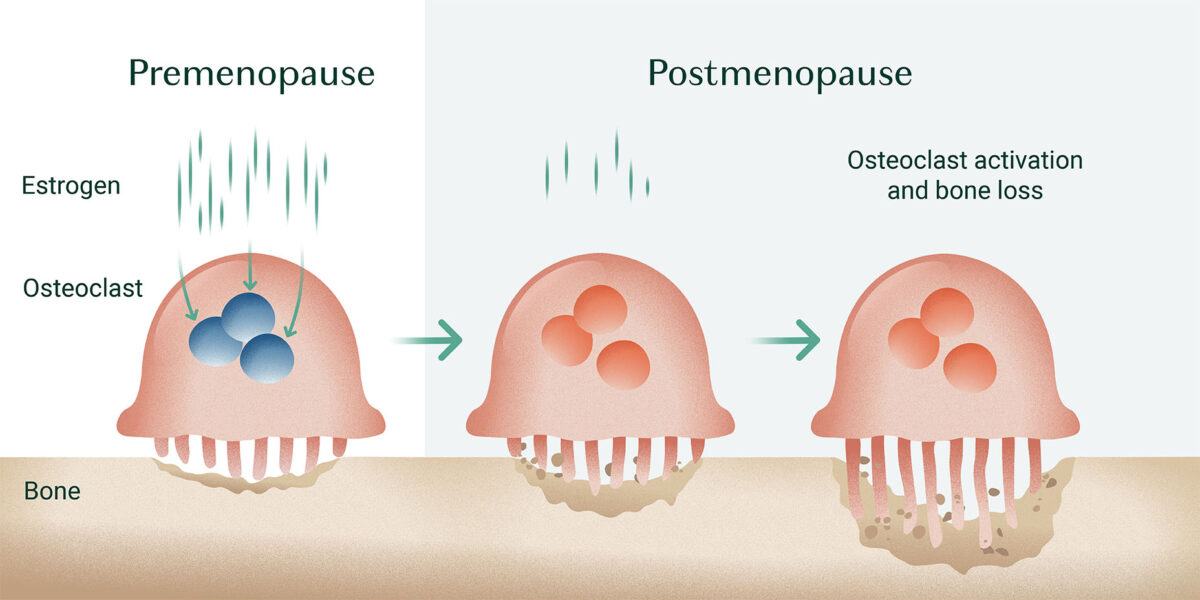
First, estrogen appears to directly target osteoclasts, inhibiting their bone-resorbing activity and inducing their apoptosis (cell death). Thereby, estrogen reduces osteoclasts’ ability to break down bone [6][7].
Furthermore, studies show that estrogen can target inflammatory molecules responsible for activating osteoclasts, another way estrogen lessens osteoclast expression [8].
In addition, estrogen has the opposite effect on osteoblast (bone-building cells) function by inhibiting osteoblast apoptosis and increasing the lifespan of these cells [9].
How to Check Your Estrogen Levels
24-Hour Comprehensive Urine Hormone Test
There are several ways to check your estrogen levels (including blood and saliva tests), but urine testing is by far the most accurate.
Throughout a 24-hour period, your hormones fluctuate significantly, meaning that the time during which you take your test will greatly impact your results. While saliva and blood tests simply provide a snapshot of your hormones during one moment, urine tests taken throughout the day can give you a more accurate view of how your hormone levels are functioning during an entire 24-hour period.
Furthermore, a 24-Hour Comprehensive Urine Hormone Test will show you your levels of 2-methoxyestradiol, a highly beneficial form of estrogen produced in your liver from estradiol. 2-methoxyestradiol protects your heart and blood vessels, has anti-cancer effects, and inhibits bone resorption. This metabolite will not be detectable in blood or saliva tests.
Interpreting Your Results: Estrogen Metabolism
Another benefit of the Comprehensive 24 Hour Urine Hormone test is that it will show you several markers that provide insight into how your body metabolizes estrogen. This will help you and your doctor determine if your estrogen metabolites are the health-promoting compounds or if you are producing some potentially dangerous ones.
Below are two markers to pay attention to:
#1 Estrogen Quotient
The estrogen quotient is the amount of Estriol (E3) divided by the sum of Estrone (E1) + Estradiol (E2). This ratio indicates how much protective, cancer-preventive estrogen you’re producing compared to the more active, potentially cancer-promoting forms of estrogen.
Your results here will appear as either an EQ<1 or an EQ>1.
- An EQ<1 indicates increased production of pro-inflammatory derivatives of estrone or estradiol called the 3,4-catechol estrogen quinones, which promote breast cancer.
- An EQ >1 indicates estrone and estradiol are being converted to protective 2-OH estrogen metabolites, indicating a lower risk of breast cancer.
Even if your lab test shows an EQ of <1, there are safe, natural, and very effective ways of improving your estriol production and correcting this.
#2 The 2/16α Ratio
The 2/16α ratio is the ratio of the protective metabolite of estrone, 2-hydroxyestrone (2-OH E1), to the super potent estrone metabolite called 16α-hydroxyestrone (16α-OH E1). The ratio of the gentle estrogen you’re producing to the potent estrogen you’re producing indicates your risk for developing breast or endometrial cancer and, if you’re a man, prostate cancer.
However, maintaining balanced levels of 16α-OH estrone is crucial for bone building. Very low levels indicate an increased risk for osteoporosis and osteopenia. Therefore, healthy levels of this marker hit the sweet spot: not too high but not too low.
The ideal 2/16α Ratio range is 2 to 4, with a ratio of <2 indicating too much 16α-OH estrone and a ratio of >4 indicating not enough 16α-OH estrone.

The good news is that this ratio is also highly modifiable with natural interventions.
Estrone’s conversion to (pro-carcinogenic) 16α-OH E1 is promoted by obesity, hypothyroidism, pesticides, alcohol, and cimetidine (the H2-blocker drug, Tagamet).
Estrone’s conversion to (protective) 2-OH E1 is promoted by:
● Cruciferous vegetables (broccoli, Brussels sprouts, cabbage, cauliflower, collard greens, kale, and turnips)
● Exercise
● Flax
● Soyfoods and, last but definitely not least,
● Omega-3 fatty acids, which we get in Triple Power Fish Oil.
Takeaway
After menopause, a woman’s ovaries stop producing estrogen, but this doesn’t mean your body no longer needs or completely stops producing estrogen in other areas. In fact, you continue to produce small amounts of estrogen in many other cells and tissues where estrogen plays critical protective roles, including in your cardiovascular system and brain, as well as your bones [10].
Therefore, even though your estrogen production will have diminished post-menopause, it’s still a good idea to check your estrogen levels, so you know how your body is metabolizing it. If you decide to utilize bio-identical hormone replacement, checking your estrogen levels and estrogen metabolites is even more essential. In either situation, you will want to know if you are producing healthy levels of bone-protective estrogen, or if you might be producing estrogen metabolites that could increase your risk for cancer? Once you know how your body is metabolizing estrogens, you can relax or gently nudge your estrogen metabolism into safe, protective metabolites.
For a complete overview of the 24-Hour Comprehensive Urine Hormone Test join the AlgaeCal Community. In the group, you’ll find lectures and printable PDFs covering this and other hormone tests.
FAQ
How does low estrogen affect bone density?
Estrogen plays a role in promoting osteoblast activity and inhibiting osteoclast production and activity. Therefore, when estrogen is low, the inhibition of osteoclasts declines, creating more bone resorption, while the promotion of osteoblast activity also declines, reducing bone rebuilding.
What is the difference between estrone and estradiol?
Estrone is the primary active form of estrogen once we are postmenopausal, while estradiol is the primary form of active estrogen during women’s reproductive years
What should estrogen levels be in postmenopausal women?
Normal levels of estradiol are 0 to 30 pg/mL for postmenopausal women. Estrone levels are in the range of about 14 to 103 pg/mL.





Donnu DelForno
August 23, 2023 , 6:31 pmHow do you significantly boost up your estrogen levels?