Yes, you do! If your healthcare provider has recommended a DEXA scan, that means he’s worried about your bones—and here’s why…
When we’re young, our bones are packed with minerals. That’s what makes them strong. But sometime after our 40th birthday, we start to lose these minerals. And every year, we lose more and more. Which makes our bones weaker and weaker.
That’s why half of all women over the age can expect to break a bone due to low bone density, according to the National Osteoporosis Foundation, all because we’re losing the minerals that make our bones healthy and strong.
A DEXA scan measures the density of these minerals in your bones, allowing your healthcare provider to determine your osteoporosis risk.
What Is a DEXA Scan?
The acronym DEXA stands for Dual Energy X-Ray Absorptiometry, and here’s how it works…
DEXAs use two X-ray beams with different energy levels that are aimed at your bones. One beam passes through soft tissue, while the other passes through your bone. The amount of radiation that passes through your soft tissue is then subtracted from the total to determine your bone mineral density. Thus, DEXA uses a “Dual Energy X-Ray [1].”
The word absorptiometry describes the amount of radiation absorbed.
Denser bones will absorb more X-ray energy as it tries to pass through, which means that if your bones have lost density, the amount of X-ray energy that passes through will be higher.
Are DEXA Scans Safe?
Bone density scans are very safe. They use a low radiation dose, so it’s not harmful. In fact, it’s about the same as the background radiation that you’d expect flying from New York to London!
Who Should Get a DEXA Scan?
The National Osteoporosis Foundation recommends that you should a DEXA scan if [2]:
- You are a woman age 65 or older
- You are a man age 70 or older
- You break a bone after age 50
- You are a woman of menopausal age with risk factors
- You are a postmenopausal woman under age 65 with risk factors
- You are a man age 50-69 with risk factors

Am I At Risk For Osteoporosis?
There are many factors that contribute to bone loss and osteoporosis. Some of these are outside your control.
Gender: Osteoporosis is more common among women because they have smaller bones and lose estrogen during menopause. Estrogen is key in maintaining bone density, so when its levels fall, the rate of bone loss increases. In fact, studies show that in the five to seven years following menopause, a woman can lose up to 20% of her bone density [3].
Age: By the time most people celebrate their 40th birthday, they’ve already begun to lose minerals from their bones. In fact, most people lose around 1% of their bone mineral density per year. This doesn’t sound like much, but it really adds up. By the time you’re 50, you’ve already lost at least 10% of your bone-strengthening minerals. Imagine a house that was missing 10% of its bricks! [4].
Family History: You’re more likely to have osteoporosis if you have a family history of osteoporosis or if one of your parents has broken a hip[5].
Osteoporosis is Underdiagnosed
About 10 million Americans have osteoporosis, and 34 million more are at risk, but the weak bones that characterize the condition often go unnoticed until they fracture, most frequently in the hip, spine or wrist. Among the older people most susceptible to osteoporosis, this can present major problems. “The gravity of fractures is often underappreciated when in fact, patients with hip fractures go on to have deterioration in their health linked directly to their fractures, with a high probability of death or nursing home placement,” according to a report from Stanford University School of Medicine.
And yet, despite the serious implications, osteoporosis is woefully underdiagnosed [6,7]. This underdiagnosis was highlighted in a 2021 study involving 235 subjects who had suffered vertebral fractures. Astonishingly, nearly 29% of these people had not been diagnosed with osteoporosis before their fracture occurred. This finding underscores the gap in early detection and diagnosis of osteoporosis, which is crucial for preventing such fractures.[14]
Despite the clear link between fractures and osteoporosis, many patients don’t receive a diagnosis for the latter, even after suffering a fracture. [8] The main reason for this is a lack of follow-up testing by healthcare providers. For instance, a study revealed that only 9% of women underwent bone mineral density tests six months after experiencing a fracture. [9]
This underscores the need to advocate for your own bone health. If you believe you might be at risk for osteoporosis or have suffered a fracture, it’s important to discuss the possibility of a DEXA bone density scan with your doctor.
Please Don’t Wait Till You’re 65 For A Scan!
At AlgaeCal, we meet many people in their 50s, 40s, and even 30s who waited too long for a DEXA scan and are surprised to discover they have low bone density. Why wait until 65 to find out? DEXA scans, a critical tool for assessing bone health, are affordable and accessible, typically ranging from $70 to $200. And many clinics offer them without requiring a doctor’s prescription. Investing in your health sooner rather than later allows you to take proactive steps toward bone strength and longevity. Don’t wait for a fracture to tell you what a simple test could have revealed.
What Happens During a DEXA Scan?
DEXA scans are painless, non-invasive procedures. When you go in for your scan, the radiographer ( a specialist taking X-ray images) will have you lay on your back on a flat, open X-ray table. During the scan, you’ll want to be as still as possible to ensure the clarity of the images, with most scans only lasting between 10 and 20 minutes.
As you lay on the table, a large scanning arm will be passed over your body to measure bone density in various areas. In most cases, your hips and lower spine will be evaluated for density if you’re checking for osteoporosis [10].
What Do My DEXA Results Mean?
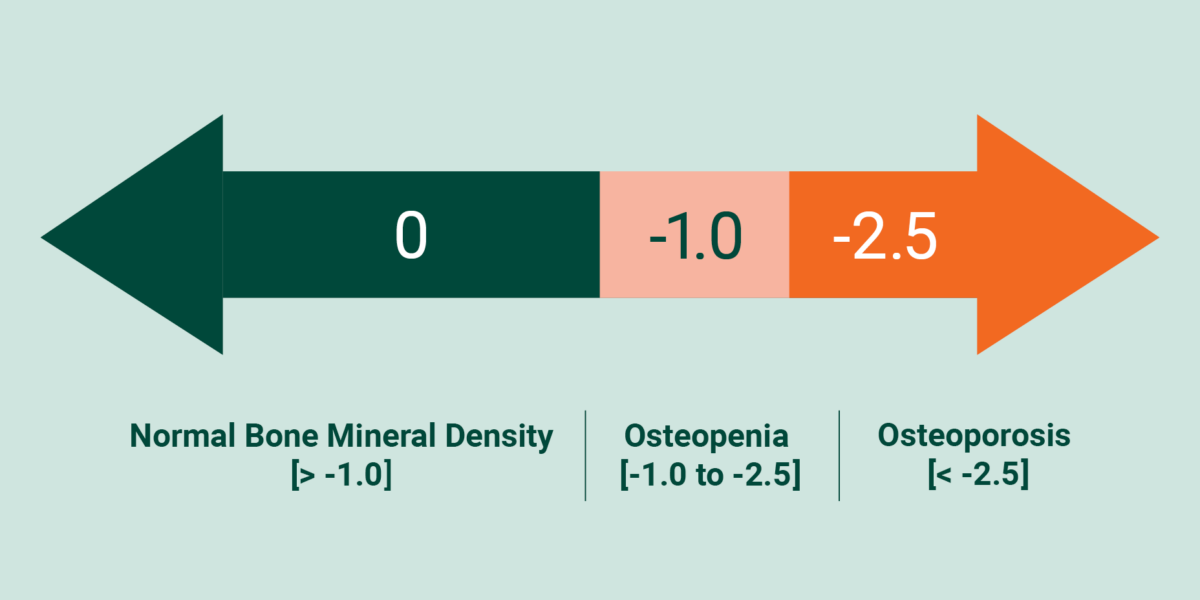
Your T-Score represents the difference between your current bone mineral density and that of a healthy young adult. Simply put, it measures your current bone mineral density against someone in the prime of their bone health. This score allows your doctor to determine if your bones are still in good shape if they’re beginning to lose density and you’re entering a phase of osteopenia, or if you are already dealing with osteoporosis [11].
- If your T-score is greater than -1.0, your bones are considered normal.
- If your T-score is between -1.0 and -2.5, your bone mineral density is below normal, and you are diagnosed with osteopenia. Left untreated, osteopenia may lead to osteoporosis.
- If your T-score is -2.5 or less, then you will be diagnosed with osteoporosis.
In addition to your T-score, your report will also provide a Z-score. The Z-score measures your bone mineral density against the average bone mineral density of someone your age and gender. This number helps you see how you’re doing compared to others in your age range. Generally speaking, a T-score is more useful for older folks, while a Z-score is used to determine bone health in children and young adults.
I Take Calcium! Do I Still Need A DEXA Scan?
Many people assume calcium protects them from bone loss. So they load up on calcium-rich foods, stock their refrigerator with calcium-fortified drinks, and even take a good-quality calcium supplement. But it doesn’t work…
That’s because bone loss isn’t a loss of calcium – it’s a loss of all the minerals that collectively hold your bone together. In fact, clinical studies show that it takes a total of 13 minerals and 3 vitamins to make your bones stronger.
So if your calcium supplement contains only calcium, you’re getting just one of the 16 nutrients needed for bone health— you’re 15 nutrients short! And without those missing ingredients, you can’t increase the density of your bones. It’s like trying to bake a cake with nothing but flour!
Remember, the technicians at your DEXA scan aren’t testing your bone calcium density – they’re testing your bone mineral density.
You don’t need more calcium. You need more minerals.
In fact, your bones need a precise combination of 13 different minerals. A combination shown in clinical trials to increase bone mineral density– even for people in their mid-80s!
In addition to calcium, she needed magnesium, boron, copper, manganese, silicon, strontium, nickel, phosphorus, potassium, selenium, vanadium, and zinc.
And if you’re going to protect and rejuvenate your weakening bones, you’ll need all these minerals – not some of them.
Besides these minerals, you also need specific amounts of vitamin D3, vitamin C, and vitamin K2-7.
That’s a lot of ingredients! But lacking even a single one of these nutrients can lower your bones’ mineral density. Leaving you weak and vulnerable to a fracture. A fracture that could cause unnecessary pain and expense laid up in the hospital … force you to give up your favorite hobbies … and even land you in a nursing home.
So What Makes A Good Calcium Supplement?
Made From Plants, Not Rocks.
Plant-based calcium is easier on your digestive system. It gives your body the calcium it needs in a form it understands – food.
Contains All The Bone-Building Nutrients, Not Some Of Them
The best calcium supplements contain all the minerals and vitamins needed to build up your bones’ mineral density.
Clinically Supported To Improve Bone Health
You can’t afford to waste time or money on something that won’t work. So only take calcium supplements that have been shown to work in published clinical trials. Now, there is only one nutritional supplement in the world that ticks all those boxes. It’s the AlgaeCal Bone Builder Pack, and it’s the only natural way to stop bone loss for good.

Takeaway
With a silent disease like osteoporosis, it can be hard to catch the signs that something isn’t quite right with your bones. Mostly because there often aren’t any signs.
That’s why diagnostic testing is the best way to ensure that your bone health is where it needs to be. Keep in mind that osteoporosis is significantly underdiagnosed, and many people don’t realize they’re dealing with weak bones until they have a fracture. Even still, some people with a fracture may remain undiagnosed, setting them up for future breaks.
Talk to your doctor about whether or not a DEXA scan is right for you, and trust your gut if you think it’s time to look at your bones. Self-advocating may be the difference between undiagnosed osteoporosis and healthy, strong bones as you age.
Sign up for the AlgaeCal Newsletter to stay updated on all things bone health and healthy aging.
FAQs
Does a DEXA scan show arthritis?
Arthritis won’t show up on a DEXA scan; instead, regular X-rays are used to diagnose arthritis. With that said, advanced osteoarthritis may appear as higher density on a DEXA scan due to potential disc narrowing.
Who should not have a DEXA scan?
While DEXA scans are generally safe, caution is advised for pregnant women or anyone who has received gastrointestinal contrast or radionuclides.
What else do healthcare providers use DEXA scans for?
In addition to bone density, DEXA scans can be used to measure body composition, such as fat and muscle mass.





Zita Marisa Mendes
July 25, 2024 , 6:59 pmmy T-score -2.7im 65yo.