Lara Pizzorno is the author of “Your Bones: How You Can Prevent Osteoporosis and Have Strong Bones for Life – Naturally” and a member of the American Medical Writers Association with 29 years of experience specializing in bone health.
Recently we asked Lara if she would help us provide a series of short, ongoing videos to help you (our customers and readers) stay up to date on the latest facts and science related to bone health.
In this latest video, Lara discusses the consequence of bariatric surgery: how it reduces your ability to absorb nutrients. Watch the video below (or read the transcript provided) and let us know what you think in the comments. 🙂
Hello, my name’s Lara Pizzorno. I’m the author of “Your Bones”, and I’m here today to share with you some information that I hope will help you to have healthier bones.
In the video prior to this one, we began talking about bariatric surgery, which is surgery to treat obesity, because these surgeries are increasing greatly as the rate of obesity in the population increases greatly. And they have very negative effects on bone that are not being well reported yet. So I wanted to share with you some information about them in hopes that if you’ve had bariatric surgery or are considering it, you can share this information with your doctor, and lessen the negative effects on your bones from these procedures.
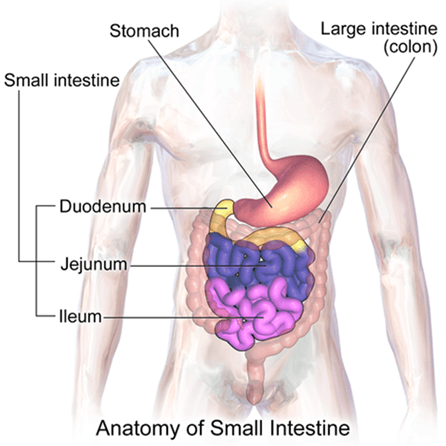
So in this video I would like to talk with you about why the Roux-en-Y and the sleeve gastrectomy, which are the two most popular forms of bariatric surgery, reduce not just the size of the stomach and thus the amount of food that we can eat, but our ability in our digestive tract to absorb nutrients. To make this easier to see I’ve sent in some diagrams of the way that the digestive tract looks normally and then what happens to it in both the Roux-en-Y and the sleeve gastrectomy procedures. And I hope these are posted along with this video.
Normal Digestive Tract
Let’s talk about the Roux-en-Y procedure first.
The Roux-en-Y surgical procedure reduces the stomach to a tiny gastric pouch that is created from about 5% of the former stomach, and is able to hold only about one ounce.
It then bypasses the first two sections of the small intestine, which are called the duodenum and the proximal jejunum. And these are the sites where virtually all active calcium absorption occurs. If you’ve read “Your Bones”, or tuned in for some of my other videos you may remember that we absorb calcium both actively and passively in our small intestines.
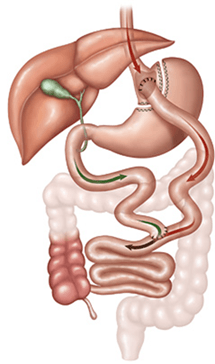
Route-En-Y
The passive portion, which takes place in the small intestine which is called the ilium, accounts for just a tiny fraction of the amount of calcium that we actually absorb normally. Active absorption is our primary means of absorbing calcium. This takes place in the first section of the small intestine, the duodenum, which is also where we absorb iron, folate, and the majority of vitamins and minerals. The important point to underscore here is that the Roux-en-Y gastric bypass bypasses the duodenum.
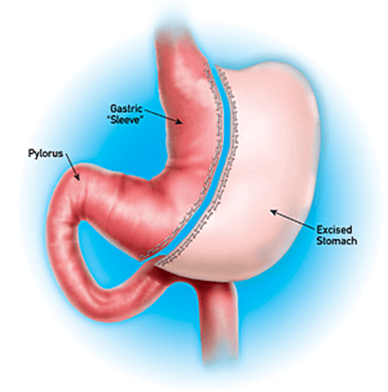
Sleeve Gastrectomy
The other procedure, the sleeve gastrectomy, is also a surgical procedure. It removes a large portion of the stomach along its greater curvature which is called the fundus. This leaves a sleeve or tube-like structure that looks like a banana and is only about 15% of the original stomach’s size.
Sleeve gastrectomy thus reduces by 85% the amount of food that it takes to fill the stomach and thus also reduces by at least 85% the amount of nutrients that can be provided by the food that we eat.
I say at least because by removing the outside curvature of the stomach, the fundus, both the Roux-en-Y and the sleeve gastrectomy greatly diminish digestive function in what is left of the stomach. This is because the fundus contains what are called the roux-guy [SP].
These are folds that help the stomach expand when we eat food, but they also contain several specialized cells that are very important for digestion, and these include our parietal cells which produce stomach acid, and our chief cells which produce pepsin, an enzyme that breaks down protein in the food that we consume. By removing the fundus, both the Roux-en-Y and the sleeve gastrectomy also eliminate all our stomach acid. It’s called hydrochloric acid, all our stomach acid producing parietal cells, which are found only in the fundus and whose job is to produce the stomach acid we need that is required to digest our food and to render calcium available for absorption. You may remember from some of my other videos that calcium requires the action of stomach acid to become solubilized which renders it able to be absorbed.
In addition, our parietal cells produce a compound called intrinsic factor, and this compound, intrinsic factor, is required for us to be able to absorb vitamin B12, which is supposed to happen in the final section of the small intestine. But intrinsic factor is produced in the duodenum, the first section, and this is bypassed in gastric bypass surgery. If you’ve read “Your Bones”, you know that B12 along with B6 and foley, played a very important bone protective role.
Without these B vitamins, a substance called homocysteine builds up inside our cells until it spills out into the blood stream and goes everywhere, including to our bones.
You can think of homocysteine as a terrorist with an acid spray gun. It damages everything it comes into contact with, greatly increasing inflammation and therefore activating osteoclats, which are the specialized cells that break down bone.
Gastric bypass surgery also eliminates our ability to absorb the fat soluble vitamins, which include vitamin D and vitamin K.
We must have vitamin D to absorb calcium. We must have vitamin K to put calcium into our bones. Normally we absorb these vitamins with the help of bile, which is produced to the liver and sent to the gallbladder from which it exits into the duodenum, the part of the small intestine right below the stomach that is bypassed in gastric bypass surgery. Bile acids are used also to produce these tiny fatty fat and water combinations which are called micelles, which are spelled M-I-C-E-L-L-E-S. Micelles are absolutely essential for the absorption of the fat soluble vitamins. Vitamins A, E, D and K. And for us to absorb fats, including the Omega 3 essential fatty acids.
These special fats, the Omega 3s which are found in our diet in the largest amounts in cold water fish like salmon and sardines, and in free range eggs, are highly anti-inflamatory and they protect not only our bones, but our brain and our blood vessels and our heart.
The sections of the small intestine where we absorb fat soluble vitamins like D and K, and these essential fatty acids with the help of bile, are bypassed in the Roux-en-Y gastric bypass surgery. Given these effects of the Roux-en-Y gastric bypass and sleeve gastrectomy on our ability to absorb necessary nutrients, at this point you may be wondering why would anyone want to have bariatric surgery? There are actually still a lot of good reasons why, and I will discuss them with you in our next video. I hope you’ll tune in. Thanks.
Sources:
Bal BS, Finelli FC, Shope TR, et al. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012 Sep;8(9):544-56. doi: 10.1038/nrendo.2012.48. Epub 2012 Apr 24. PMID: 22525731
Medical Physiology,2nd edition, eds.Walter F. Boron MD PhD, Emile L. Boulpaep MD, Saunders/Elsevier: Philadelphia, 2008.
Obesity facts, figures and guidelines. West Virginia Division of Health Statistics accessed 3-6-15 http://www.wvdhhr.org/bph/hsc/pubs/other/obesity/commor.htm





Sue
March 1, 2022 , 11:23 amI am looking for ways to assist with vitamin absorption. I am 5 years out from roux-en-y surgery and I am just now fully understanding that my body doesn’t absorb all of the nutrients that are put into it. My ferritin levels are very low and I am symptomatic. I want to get a firm handle on my health before mstters get worse. Are there partucular foods, vitamins, minerals and/or enzymes that you would suggest to help ensure absorption? My weight is no longer an issue, my health is. I appreciate any guidance you may be able to offer.