The effect leukemia has on the bones of cancer patients has been studied by researchers at the University of Rochester and a new perspective which is both thought-provoking and has surprise element to it has been arrived at. The study further sparks potential that therapies which treat bone disorders could aid in the treatment of leukemia. It also lays the foundations of a possible path that newly diagnosed leukemia patients be screened for osteoporosis. (1)
Leukemia is a form of blood or bone marrow cancer in which there is an abnormal increase in the production of white blood cells. According to the Leukemia Research Foundation approximately 74,000 people in the U.S will have leukemia diagnosed for them out of which 21,000 may die of the disease. (2)
Blood stem cells are multi-potent in nature and give rise to all types of mature blood cells like myeloids (monocytes, erythrocytes, platelets, neutrophils etc) and lymphoids (T cells and B cells etc). This allows for both self-renewal/repair and expansion.
Studies in 2003 had noted that bone cells called osteoblasts which worked in the same microenvironment as the blood stem cells were responsible for the production of bones were possibly involved in the expansion and support required during the production of normal blood cells.
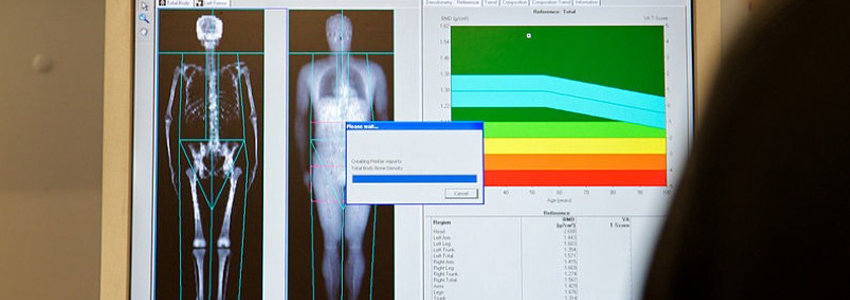
In the study that was conducted by the researchers at the University of Rochester, it was found that even in the very early stages of leukemia when cancer cells are not detectable in the blood, the leukemia cells entrenched themselves in the bone marrow and destabilised the production of healthy blood stem cells.
Until now, there had been no definition of the critical interactions that take place between leukemia cells and osteoblasts and osteoclasts (bone cells responsible for bone breakdown). However, the new research showed (on the mouse model) that leukemia cells affect the balance and the cycle of osteoblast-osteoclast activity. This alteration of the tightly-knit balance was found to be complex process and eventually caused quantifiable changes to the human skeleton. One would intuit that this was caused due to a marked increase in production of osteoclasts, but it was found that there was only a mild increase in osteoclasts responsible for bone resorption. What did happen however was that there was a more significant suppression of the production of osteoblasts (bone forming cells). In such and other ways, leukemia uncoupled these two bone cell functions. (3)
Another observation was that the way in which the bone marrow microenvironment was affected due to the presence of leukemia cells, slowed down the recovery of a person post-chemotherapy. It was suspected that the disturbance in the microenvironment may also be the potential cause to instigate a relapse of leukemia.
The good news was that the preliminary laboratory experiments on mice with leukemia demonstrated that treatment with anti-resorptive drugs restored some of the bone loss. (4)
According to Calvi, MD and associate professor in the Department of Medicine at the University of Rochester, “Our findings are quite provocative and we hope they will lead to new approaches to promote normal blood production in patients with blood cancers. Because the loss of normal hematopoietic function is the chief cause of serious illness and death among leukemia patients, it is critical that we understand all aspects of how this occurs and find new strategies to accelerate the recovery of these defects.” (1)
SOURCES:
- Leukemia Cells Are ‘Bad to the Bone’, Research Finds; Science Daily News; February 2012; http://www.sciencedaily.com/releases/2012/01/120126161129.htm
- Leukemia Statistics; Leukemia Research Foundation; February 2012; http://www.leukemia-research.org/page.aspx?pid=214
- URMC Finds Leukemia Cells Are “Bad to the Bone”; University of Rochester Medical Center Newsroom; February 2012; http://www.urmc.rochester.edu/news/story/index.cfm?id=3399
- Functional Inhibition Of Osteoblastic Cells In An In Vivo Mouse Model Of Myeloid Leukemia; Blood (Journal); February 2012; http://bloodjournal.hematologylibrary.org/content/119/2/540
- Bad to the bone; Blood (journal); February 2012; http://bloodjournal.hematologylibrary.org/content/119/2/323




Article Comments