Obesity is a global epidemic, and a well-known risk factor for several health conditions, including metabolic syndrome, heart disease, and diabetes. But what about the health of your bones? Can excess weight increase risk for osteoporosis and fracture?
It turns out the answer may not be so simple, but we’re going to explore the research and highlight what you need to know about weight, bone health, and the potential risk of osteoporosis and fracture.
Is Obesity a Risk Factor For Osteoporosis?
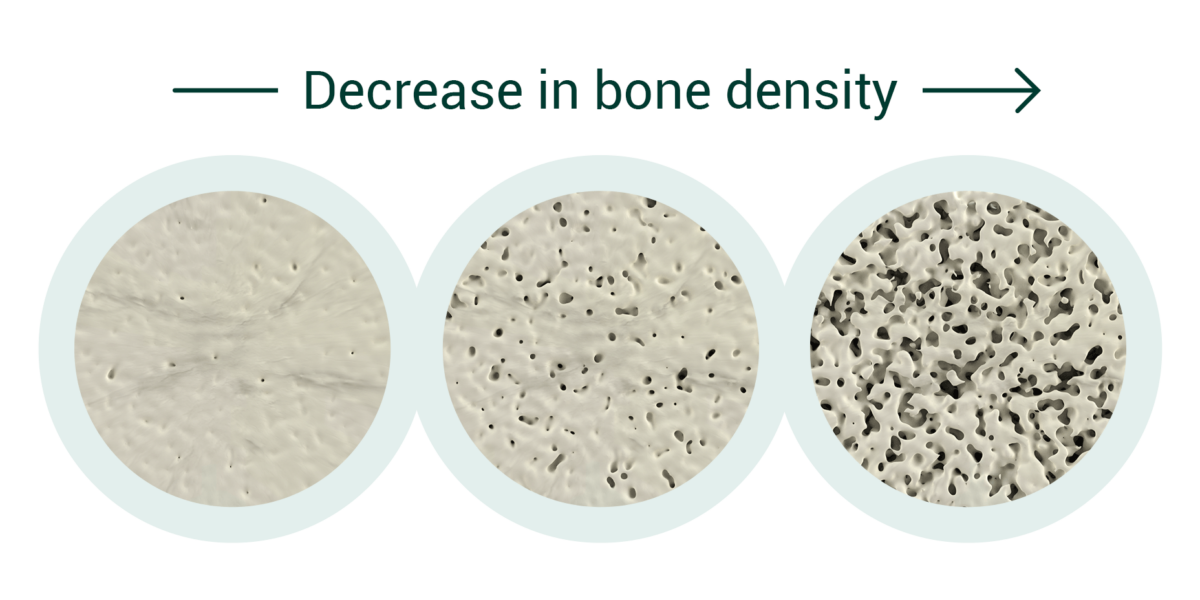
Osteoporosis is a condition that weakens bones, making them fragile and more likely to break. It affects millions of people worldwide, is more common with age and with unfavorable lifestyles such as lack of exercise.
There’s been some controversy in the research world regarding the connection between obesity and osteoporosis.
Historically, it was believed that obesity may actually be preventative against osteoporosis due to the effect of increased mechanical stresses excess body mass can place on the skeleton. It has also been suggested that the extra fat tissue may help prevent certain fractures, providing cushioning on falls.
However, a growing body of research shows that obesity is a risk factor for fracture [1]. Why might that be?
While it’s true that mechanical stress to your bones may enhance bone strength, it turns out that the impact of obesity isn’t so simple. Due to several factors (to be discussed below), obesity may reduce the quality of your bones and therefore set the stage for osteoporosis and other bone-related issues. Trabecular bone score (TBS) is an index of bone microarchitecture (quality) of bone. Researchers have found reduced TBS in obese individuals despite a normal bone mass [2, 3]. In fact, studies also show that bone strength is not proportionate to body mass in overweight and obese children and adults [4, 5, 6] and there is a higher risk of certain fractures [6, 7, 8].
Now, let’s dive a little deeper into what the research can tell us about how obesity may undermine bone health.
How Does Obesity Affect Bone Health?
Like everything else in the body, the relationship between bone and fat tissue is complex. While researchers haven’t nailed down one specific mechanism for the relationship between obesity and osteoporosis, several factors likely play a role.
The relationship between bone and excess fat tissue is complex. It is likely there is more than one specific mechanism for the link between obesity and osteoporosis, including the following:
#1 Inflammation
Obesity is associated with low-grade, chronic inflammation, characterized by higher levels of inflammatory compounds that may interact with the different tissues in your body [4, 9]. Studies show that chronic inflammatory conditions of almost any cause, can lead to bone loss due to the interaction that inflammatory compounds have on bone cells. Specifically, studies show that in an inflammatory environment, osteoclast (cells that break down bone) activity increases, while osteoblast (bones that build up bone) activity decreases. As a result, chronic inflammation can lead to alterations in bone metabolism and as a result, net bone loss [9].

#2 Low Levels of Adiponectin
Another potential culprit behind the obesity-osteoporosis connection is a hormone called adiponectin. Adiponectin is a hormone that’s produced by fat cells (adipocytes) and tends to be lowered in obese individuals. In one study, postmenopausal women with metabolic syndrome showed significantly lower adiponectin levels along with lower bone density when compared with healthy controls [10].
What exactly is the connection between adiponectin and bone density? In an animal study, investigators found that mice deficient in adiponectin displayed signs of osteoporosis. When they dug deeper, they found that stem cells in these mice preferentially differentiated into fat cells as opposed to bone-building osteoblast cells. These results indicate that adiponectin plays a role in the formation and function of bone-building cells. Since obese individuals tend to be lower in adiponectin, their stem cells may be primed to turn into fat instead of bone[11].
#3 Vitamin D Deficiency
While inflammation and hormones likely play a role in the connection between obesity and osteoporosis, we can’t forget about the role of micronutrients.
It’s well understood that vitamin and mineral deficiency can set the stage for osteoporosis. The strength of your bones relies on adequate mineralization and nutrients like vitamin D help to manage those minerals and ultimately usher them into your bones.
Unfortunately, studies show that in overweight individuals, there is an inverse relationship between active vitamin D and body weight. In fact, research suggests that serum concentrations of vitamin D may be 20% lower in obese individuals than in those of a healthy weight[12].
Without adequate vitamin D, your bones cannot absorb the minerals (particularly calcium) they need to become strong and healthy. Over time, low levels of vitamin D may lead to a loss in bone density and, ultimately, osteoporosis[13].

#4 Sedentary Lifestyle – Use it or Lose it!
A sedentary lifestyle can lead to obesity, because the body takes in more calories than it burns during energy expenditure, and the excess calories are converted and stored as excess fat. Having a sedentary lifestyle also means that bones do not receive the mechanical stimulus they need to maintain their strength [14]. When this happens, bone consequently becomes weaker. This can also be seen in anti-gravity, with astronauts losing TBS and BMD during space missions [15]. Weight-bearing and muscle strengthening exercises are important for building bone strength and preventing osteoporosis. The phrase “Use it or Lose it” is just as important for bone as it is for muscle.
Takeaway
As you’ve learned, evidence suggests that the hormonal, nutrient, and inflammatory conditions are implicated in the link between obesity, osteoporosis and fracture.. While research continues in this area, it’s clear that maintaining a healthy weight is an important step for protecting bone health.
On the flip side, studies also indicate that being underweight may pose risks for bone density as well. Having a Body Mass Index (BMI) below the healthy threshold is associated with reduced bone strength and an increased risk for fracture.
The solution? Do your best to find a weight that’s healthy for you. Adding weight-bearing and/or muscle-strengthening exercise to your routine can enhance weight loss efforts while increasing bone strength, and ensuring your diet is nutrient-rich will assist you in getting the micronutrients you need for both metabolic and bone health.
For more tips on healthy living, sign up for the AlgaeCal Newsletter.
FAQs
Are obese people more likely to have osteoporosis?
Obesity may increase the risk for osteoporosis and fracture due to factors such as inflammation, hormonal imbalances, nutrient deficiencies and sedentary lifestyle.
How does obesity affect bone density?
Some mechanisms by which obesity may affect bone density include increased inflammation, disruption of hormones, and deficiencies in nutrients like vitamin D.
Will losing weight help osteoporosis?
It’s possible that losing weight may assist in reducing your risk of osteoporosis by lowering your body’s inflammation, correcting hormonal imbalances, and assisting with nutrient deficiencies. It is important to include exercise that will also strengthen bones and muscle.
Do heavier people have stronger bones?
People with excess weight may have higher bone density but this is not proportional to their higher body mass. Also, metabolic factors that come with obesity and being overweight may reduce bone quality, which may lead to weaker bones and a higher risk of certain fractures.






Theresa Beville
September 9, 2023 , 4:48 pm1)Does Ozempic for weightloss (without diabetes) to treat obesity with a B.M.I. of 33 adversely affect osteoporosis?
2)Does diverticulitis affect osteoporosis?
3)Does COPD affect osteoporosis?
4)Can algae-cal offset any adverse effects of the use of Ozempic for obesity?